Why America's Ebola patients survive
Thousands are dying from the viral disease in Africa. Why are patients treated in the U.S. recovering?

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
What is Ebola's mortality rate?
It largely depends on where patients are treated. In the current outbreak in West Africa, about 70 percent of the 13,000 people infected have died. But of the nine confirmed cases in the U.S. — a mix of medical volunteers who returned from Liberia, Guinea, and Sierra Leone and the health workers who caught the disease treating them here — there has been just one fatality: Liberian national Thomas Eric Duncan. Eight patients were successfully treated and discharged, including Dr. Craig Spencer, who left Bellevue Hospital in New York City this week. Thus far, the mortality rate of Ebola patients treated in the U.S. is 11 percent, and it might be zero had Duncan's treatment not been delayed because of a misdiagnosis when he first went to the hospital in Dallas. An Ebola infection is "not a death sentence," says Michael Buchmeier, a virologist at the University of California at Irvine. "It's a beatable disease."
Why is treatment in the U.S. working?
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
American hospitals have superior facilities, equipment, and staffing. When a patient starts suffering from severe vomiting and diarrhea, it is imperative that his or her lost fluids — up to 5 gallons a day — are replenished via an IV drip, to prevent organ failure and shock. Doctors here are well equipped to do that, and can also carefully monitor and adjust electrolyte levels in the blood — chemicals such as potassium, magnesium, and sodium — that can plummet with fluid loss. In a Liberian field hospital, IV lines, saline solution, and monitoring equipment are in short supply. American physicians have also had access to the experimental antiviral drug ZMapp, and blood serum from patients who've developed antibodies to Ebola. They can use a huge array of drugs for treating other symptoms, such as abdominal pain and low blood pressure. If necessary, doctors can bring in ventilators and dialysis machines to keep struggling patients alive long enough for their immune systems to fight off the disease.
What about staffing levels?
In the U.S., there are 245.2 doctors per 100,000 people; in Liberia, it's just 1.4, or about 60 in total. So when Rick Sacra, a missionary, was being treated for Ebola in Liberia, he saw a doctor only once a day. But after being evacuated to the Nebraska Medical Center — one of four U.S. hospitals with biocontainment units designed for treating infectious-disease patients — he received round-the-clock care from more than 40 highly trained health workers, including a nurse permanently stationed in his room. None of this came cheaply; insurance companies estimate that treating an Ebola patient can cost up to $25,000 a day. In Sierra Leone, where annual health-care spending is just $205 per capita, that level of care is not possible. "There's no magic going on," says infectious-diseases expert Dr. Bruce Farber. "The supportive care in the U.S. is just incredibly different."
How else is it different here?
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
Most of the U.S. patients began treatment at the first sign of infection. In West Africa, so many patients have died in Ebola treatment centers that people fear them and thus do not get medical help until they're gravely ill — at which point their organs are failing and the viral load is too large for their bodies to fight off. American hospitals are also much better at preventing the spread of infection to their health workers. When Atlanta's Emory Hospital became overwhelmed by the amount of Ebola-contaminated waste, it immediately installed an industrial-size autoclave, which uses pressure and 275-degree heat to sterilize any kind of material. Field hospitals in West Africa tend not to have autoclaves.
Can West African care be improved?
Yes, but it will take more equipment, facilities, doctors, and money. The U.S. is sending 3,900 troops to shore up infrastructure in the region, with the initial aim of building 17 Ebola treatment centers with 100 beds each. But it may be hard to staff them. The high infection rate among health workers — 310 have died since the outbreak began last December — is deterring foreign volunteers. Understaffing is now such a problem that only 22 percent of the planned 4,707 treatment center beds in West Africa are operational. "The personnel is a critical factor," says Dr. Gino Strada, founder of the nonprofit group Emergency. For a 100-bed hospital, he says, "you need 100 nurses and 10 to 15 doctors."
Is there any hope of a cure?
A few treatments have certainly shown promise. Patients who were given the experimental drug ZMapp, which did exceptionally well in animal trials, showed an immediate improvement; however, two of the seven recipients eventually died. Blood transfusions from Ebola survivors may have helped some patients, and researchers have begun a number of trials for potential vaccines. But until a medical breakthrough is made, the keys to fighting Ebola — on both sides of the Atlantic — are resources and manpower. "You need the four S's," says Paul Farmer, co-founder of the aid group Partners in Health: "Staff, stuff, space, systems."
Four weeks of hell
Dr. Kent Brantly's first symptom was a mild fever. By the time he tested positive for Ebola in a Liberian health-care facility a few days later, the Samaritan's Purse missionary had lost his appetite and was overwhelmed with nausea. "I didn't think, This is it, I'm dead," he said, "but it was very sobering to realize that I may die right here in my bedroom." Brantly's fever passed 104, the diarrhea and vomiting began, and the 33-year-old spent the next few days trying to stay hydrated as he lost more than 2 gallons of fluids a day. Soon, his near-continual diarrhea turned black, and his vomit turned purple — signs that the virus was damaging the walls of his blood vessels, causing internal bleeding. When he started struggling to breathe, the father of two called his wife to say goodbye. Thankfully, his farewell proved premature. After he was given a dose of ZMapp, his condition improved, and the next day he was flown to Atlanta for treatment. After 19 days in intensive care, Brantly walked out of the hospital, having beaten Ebola.
-
 Crisis in Cuba: a ‘golden opportunity’ for Washington?
Crisis in Cuba: a ‘golden opportunity’ for Washington?Talking Point The Trump administration is applying the pressure, and with Latin America swinging to the right, Havana is becoming more ‘politically isolated’
-
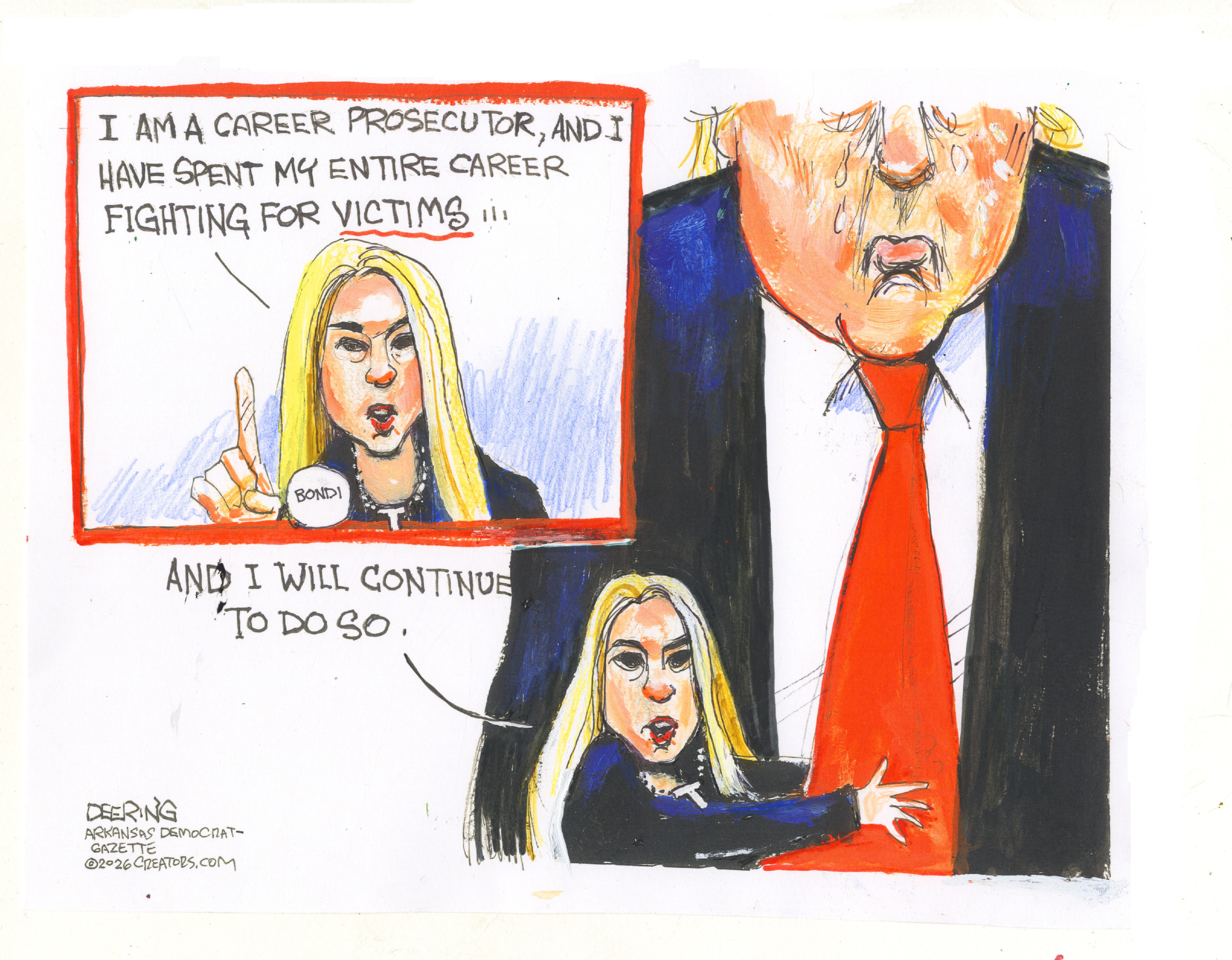 5 thoroughly redacted cartoons about Pam Bondi protecting predators
5 thoroughly redacted cartoons about Pam Bondi protecting predatorsCartoons Artists take on the real victim, types of protection, and more
-
 Palestine Action and the trouble with defining terrorism
Palestine Action and the trouble with defining terrorismIn the Spotlight The issues with proscribing the group ‘became apparent as soon as the police began putting it into practice’