Life and death on Ebola's front lines
Fired by compassion and protected by plastic, these Americans are treating the sick in Liberia

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
THE FIRST TIME Dr. Steven Hatch suited up in protective gear at an Ebola treatment center in Suakoko, Liberia, he was confronted with the weight of his decision to volunteer here. A patient, sweating and heavily soiled, had collapsed in a corridor. "Literally every surface of his body was covered in billions of particles of Ebola," he recalled.
The physician introducing him to the routine, Dr. Pranav Shetty, said they needed to get the man back to bed, so they picked him up. Shetty focused on calming the patient, who would not live through the night. He diluted a Valium tablet in water and cut some intravenous tubing into a crude straw for him to sip.
"It was a beautiful moment, because I was like, 'He's a doctor; he was taking care of his patients,'" said Hatch, an American volunteer. "That's what we do here."
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
In his first two weeks in Liberia at a new clinic run by the charity International Medical Corps, Hatch has learned the ways of the Ebola ward.
Much of West Africa is following a no-hands rule to avoid contagion from the deadly virus, but doctors and nurses here, protected by layers of plastic and rubber armor, routinely touch the sick. Without a drug that can cure the disease, they offer patients fluids and medications to treat symptoms, but also the simplest of comforts, like feeding them or cleaning them up. They follow their instincts — Hatch turned out to be right that an elderly man suffered from a chronic illness, not Ebola, as a blood test mix-up showed — but try to restrain their impulses, because old habits might not be safe.
Hatch's journey to this remote center in a tropical forest began last month at a training course run by the Centers for Disease Control and Prevention at a former Army base in Anniston, Alabama. An infectious-disease specialist in Worcester, Massachusetts, Hatch, 45, joined about two dozen other medical workers heading to West Africa.
Outside a battered warehouse at the base, with peeling walls that served as a mock Ebola treatment unit, mannequins were sprawled on the ground. Hatch and Bridget Anne Mulrooney, an American nurse who was volunteering with the same charity, spent nearly 20 minutes putting on gear: two or three pairs of gloves, aprons, head coverings, goggles, masks, and chemical protection suits that were hot and crinkled when they walked. Hatch had trouble tying a knot with the double gloves. "I was never good at surgery," he confessed.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
As Mulrooney, Hatch, and two others lifted the first mannequin onto a stretcher, an instructor watched. She warned Hatch that the edge of his mask had come out from under his goggles, leaving part of his face exposed.
"We put him down and we go straight out," Hatch told the team, his voice muffled by the mask. "Second time in two days I've breached here. Is it because I'm 6-foot-2?"
Last year, in the Liberian capital, Monrovia, Hatch had helped teach medical residents with one of the country's top physicians, Dr. Abraham Borbor. "We laughed for two weeks," Hatch said. "I just loved him."
Borbor died from Ebola in August, which spurred Hatch to join the effort his friend had begun. He signed on for a four-week rotation with International Medical Corps, a Los Angeles–based relief group that was starting its first Ebola treatment unit, with funding from the U.S. Agency for International Development.
Mulrooney, 36, was already on the charity's emergency roster. She had volunteered in other crises and had worked for four years in Haiti. After the Ebola epidemic erupted, she put off a plan to move in with her boyfriend near London. "I feel like I have something to offer," she said.
Mulrooney's first days at the treatment center were a gut punch. "This morning I carried a baby to the tent morgue," she wrote in a Facebook message. The infant had appeared to be doing well. "It was a shock and a testament to how rapidly situations can change."
She cared for a 13-year-old girl whose intravenous site would not stop bleeding. "I cleaned her up and put her in a pair of still-tagged jeans," Mulrooney wrote. "She half smiled and took some medicines I asked her to. I won't forget her smile. Nor her soft moans as her body was fading away." The nurse added, "I'm sorry for being graphic." Hatch came about a week later. He noticed Mulrooney had lost weight. "She's a different Bridget," he observed.

AT HIGH NOON the day after his arrival, Hatch was struggling. Inside his protective equipment, after only 30 minutes on the ward, his mask was wet. "It feels constantly like being pushed down, like suffocating," he said. His goggles were steaming up. He was sweating so much — the temperatures often reached more than 90 degrees outside and even more inside the ward — that he felt like he was swimming inside his suit.
He gave water to patients and cleaned them over the course of nearly two hours. "Longer than I should have been in," he said after his gear was sprayed down in bleach solution and then carefully removed. He was breathing hard.
In the unit — about 20 international medical volunteers work alongside 175 Liberian nurses, physician assistants, aides, and others in three shifts — the workers look out for one another. Monitors observe every time someone suits up to make sure steps are followed. (The center uses protocols established by Doctors Without Borders and will serve as a training site for other aid groups.) Dr. Colin Bucks, an emergency physician from Stanford, urged his colleagues to limit visits to the wards to an hour at a time; if someone passed out, safe removal of his or her garb would be nearly impossible. He switched his shifts to overlap with Hatch's.
Mulrooney serves as a motivator. "Welcome to afternoon!" she said one day, doing a little dance for a nurse who had come in on her day off. Hatch amused his Liberian colleagues by learning to sing one of their devotionals. A Liberian physician assistant, A. Welehyou Duo, rescued him from a botched blood draw; like many American doctors, Hatch had rarely done that task since medical training.
"It's teamwork," said Duo, who previously supervised a primary health center. Love Fassama, 30, a nurse assistant, said she felt compelled to help her fellow Liberians. "I can't have these skills and sit at home," she noted.
Hatch, married with 13-year-old twins, says he is at peace with his decision to treat Ebola patients. "I just don't worry about my life," he said. "When you're scared, you get jumpy. When you get jumpy, you make bad decisions."
Last Friday, he carried a malnourished 9-year-old girl, Blessing Gea, into the unit for those confirmed to have the disease. The next night, Mulrooney, clad in full protective gear, tended to the lonely little girl. She let her lean against her as she squeezed a packet of peanut butter–based supplement into the child's mouth. She changed her clothing, put new sheets on her bed, and wrapped her in a fuzzy blanket for the chilly night, stroking her head. Three days later, a blood test showed the girl had recovered from Ebola.
Hatch visited a new patient, a pastor who was gravely ill by the time he was admitted last week yet insisted on praying for the American doctor.
"To see a guy lying in bed that's got a 50-50 chance of living or dying pray for you?" Hatch said, shaking his head. The next day, just before the pastor died, he prayed for Hatch again.
This article originally appeared in The New York Times on Oct. 16. Reprinted with permission.
-
 Switzerland could vote to cap its population
Switzerland could vote to cap its populationUnder the Radar Swiss People’s Party proposes referendum on radical anti-immigration measure to limit residents to 10 million
-
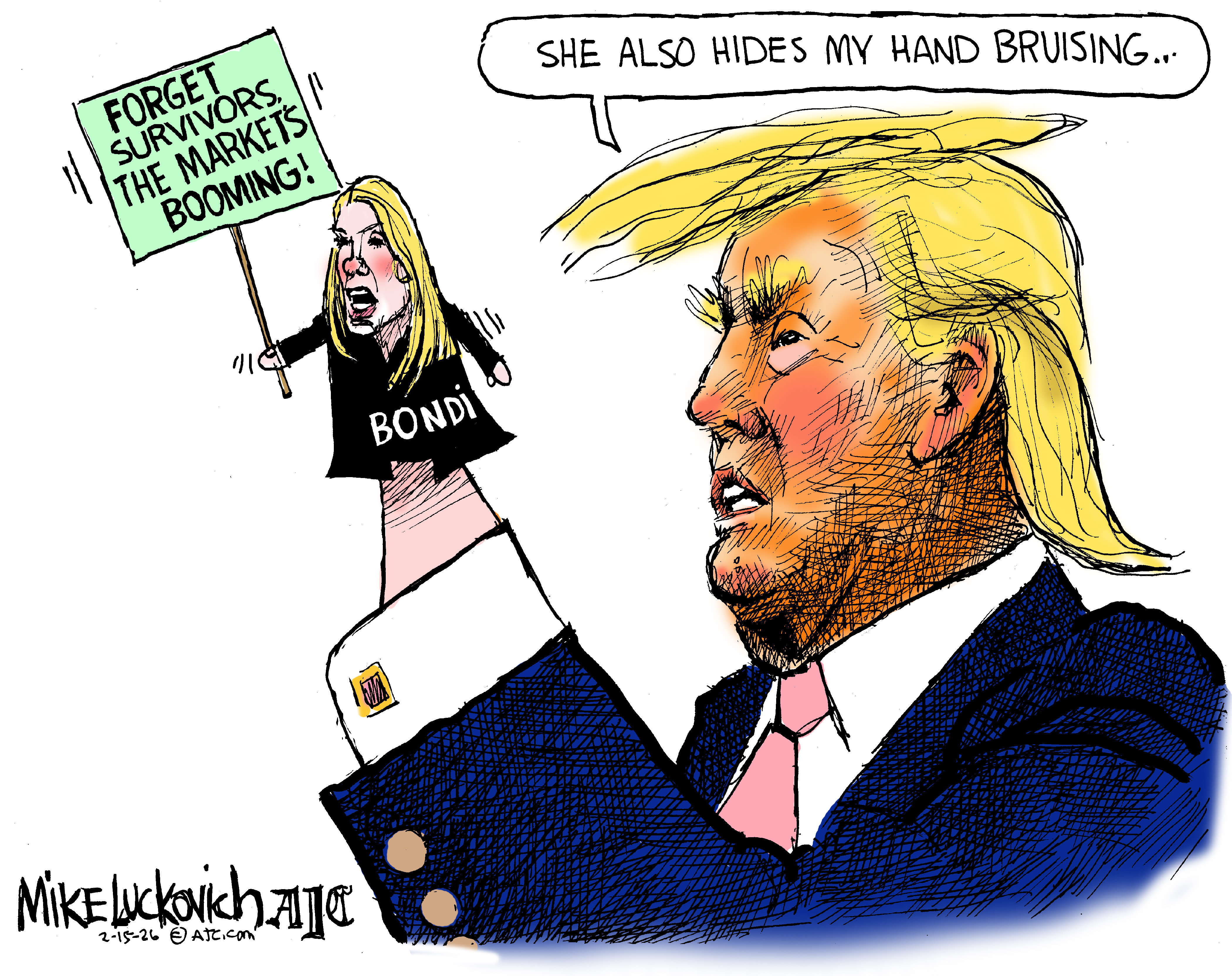 Political cartoons for February 15
Political cartoons for February 15Cartoons Sunday's political cartoons include political ventriloquism, Europe in the middle, and more
-
 The broken water companies failing England and Wales
The broken water companies failing England and WalesExplainer With rising bills, deteriorating river health and a lack of investment, regulators face an uphill battle to stabilise the industry