The nursing home disaster
How coronavirus devastated America's long-term care facilities

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Over 40 percent of U.S. coronavirus deaths have been linked to long-term care facilities. Why? Here's everything you need to know:
How bad were the outbreaks?
More than 43,000 people and at least 400 workers perished of COVID-19 in nursing and long-term care facilities. The first outbreak, which essentially launched the pandemic in the U.S., came in February at the Seattle-area Life Care Nursing facility, where two-thirds of the residents and 47 workers were infected and 37 ultimately died. As other outbreaks exploded, the Centers for Disease Control locked nursing homes down in March, and family members described the horror of being unable to reach their loved ones, in some cases only learning of a parent's illness after the patient died, surrounded by strangers in an ad hoc sick ward. Ghastly stories surfaced: At a New Jersey facility, 68 people died and 17 corpses were piled up in a morgue designed to hold four. At the Soldier's Home in Holyoke, Massachusetts, a veteran's home, at least 74 died, and the National Guard was called in to relieve the superintendent. Nationwide, overwhelmed workers, typically low- and minimum-wage, quit en masse, prompting staffing shortages. Many homes failed to alert families and public officials of outbreaks, possibly out of fear of fines or inspections.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
Why was it so bad?
For a highly infectious virus like the new coronavirus, nursing homes were like dry tinder in a wildfire. Mortality rates for COVID-19 rise dramatically for those over 70, especially if they have pre-existing conditions such as heart disease. Moreover, nursing facilities are often cramped, with multiple residents sharing a room, bathrooms, and other common areas — perfect conditions for viral spread. Aides, who often work at multiple facilities, move from room to room to provide basic, hands-on care, such as washing and repositioning of frail patients. Low Medicaid payments, said Harvard Medical School professor David Grabowski, "really compromised the ability of nursing homes to implement strong staffing and infection control practices." (About 65 percent of patients pay using Medicaid.) The federal government said recently that 82 percent of the nearly 13,300 nursing homes it inspected from 2013 to 2017 were cited for at least one deficiency in infection prevention and control. Even in May, federal inspectors who visited 6,000 facilities found "sporadic noncompliance" with CDC rules for limiting infection, including staffers not washing their hands or observing strict isolation for the ill.
Were the homes at fault?
Outbreaks were inevitable, but the industry has not complied with regulations that could have reduced the scale of the disaster. In 2016, the Obama administration introduced new regulations requiring nursing facilities to train staff on dealing with the arrival of a novel and contagious virus. Although the "all hazards rule" did not mandate the stockpiling of personal protective equipment, or PPE, homes were required to create staffing contingency plans, as well as plans for evacuating residents, sheltering in place, and getting residents food, medicine, and water during the crisis. The industry heavily lobbied against the rules, describing them as "extremely burdensome" in a letter to then newly elected President Trump. From November 2017, when the rule went into effect, to March 2020, inspectors logged more than 24,000 deficiencies in emergency plans at 6,599 nursing facilities, according to an analysis by ProPublica. "It's just a river of grief, and it could have been prevented," said Pat McGinnis, executive director of California Advocates for Nursing Home Reform.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
What role did government play?
The industry claims that even as the death toll mounted, its pleas for PPE and tests were never met. As a result, many facilities experienced lethal shortages of PPE. In the suburbs of Baltimore, one home's workers said they were given rain ponchos to protect them from infection. In East Los Angeles, a staffer said she was given swimming goggles. In New York, Gov. Andrew Cuomo (D) ordered nursing homes to accept recovering coronavirus patients from hospitals, and the Associated Press found 4,500 returned before the directive was repealed on May 10. The state suffered 5,800 nursing home deaths, more than any other. Cuomo later said he was told to send recovering COVID patients to nursing homes by the CDC and White House.
What's being done now?
On April 30, Trump vowed to "deploy every tool, resource, and power" to protect elderly Americans. In mid-May, the administration said it wanted all residents and staff tested over the ensuing two weeks. But by the end of May, more than 3,200 facilities said they still had less than a week's supply of PPE and sanitizer, and that some PPE they'd received was defective. State and federal officials had still not provided adequate testing, Vox reported. "They have not put real dollars behind it," Grabowski said. For Brenda Anagnos, whose 81-year-old mother, Carol Ballard, died at the Kimberly Hall North facility in Windsor, Connecticut, the pain is hard to reconcile. "She had life left," Anagnos said of the grandmother of four. "She didn't deserve to die like this."
Immunity from lawsuits
Governors in 20 states have issued orders shielding nursing facilities and their workers from legal liability during the pandemic. State officials insist that such action does not excuse gross negligence, and was necessary in order to ensure "maximum participation" among frontline health-care workers during a moment of crisis, as Democratic Connecticut. Gov. Ned Lamont put it. Sen. Majority Leader Mitch McConnell (R-Ky.) has vowed to include such immunity in any additional rounds of pandemic relief legislation as a means of reducing opportunistic nuisance lawsuits. Some fear the industry is trying to evade liability for problems that existed pre-pandemic. But for now, such immunity orders have troubling implications for families whose loved ones perished in long-term care facilities under uncertain circumstances. Roberta James-Brown said her father, Johnny, died at 85 from COVID-19 at a Connecticut facility on April 9. She doesn't know how, and lawyers have told her Lamont's immunity order will make finding out harder. "I don't even know if they were neglectful," she said, adding that she just wants "a clear picture of what really went on there."
This article was first published in the latest issue of The Week magazine. If you want to read more like it, you can try six risk-free issues of the magazine here.
-
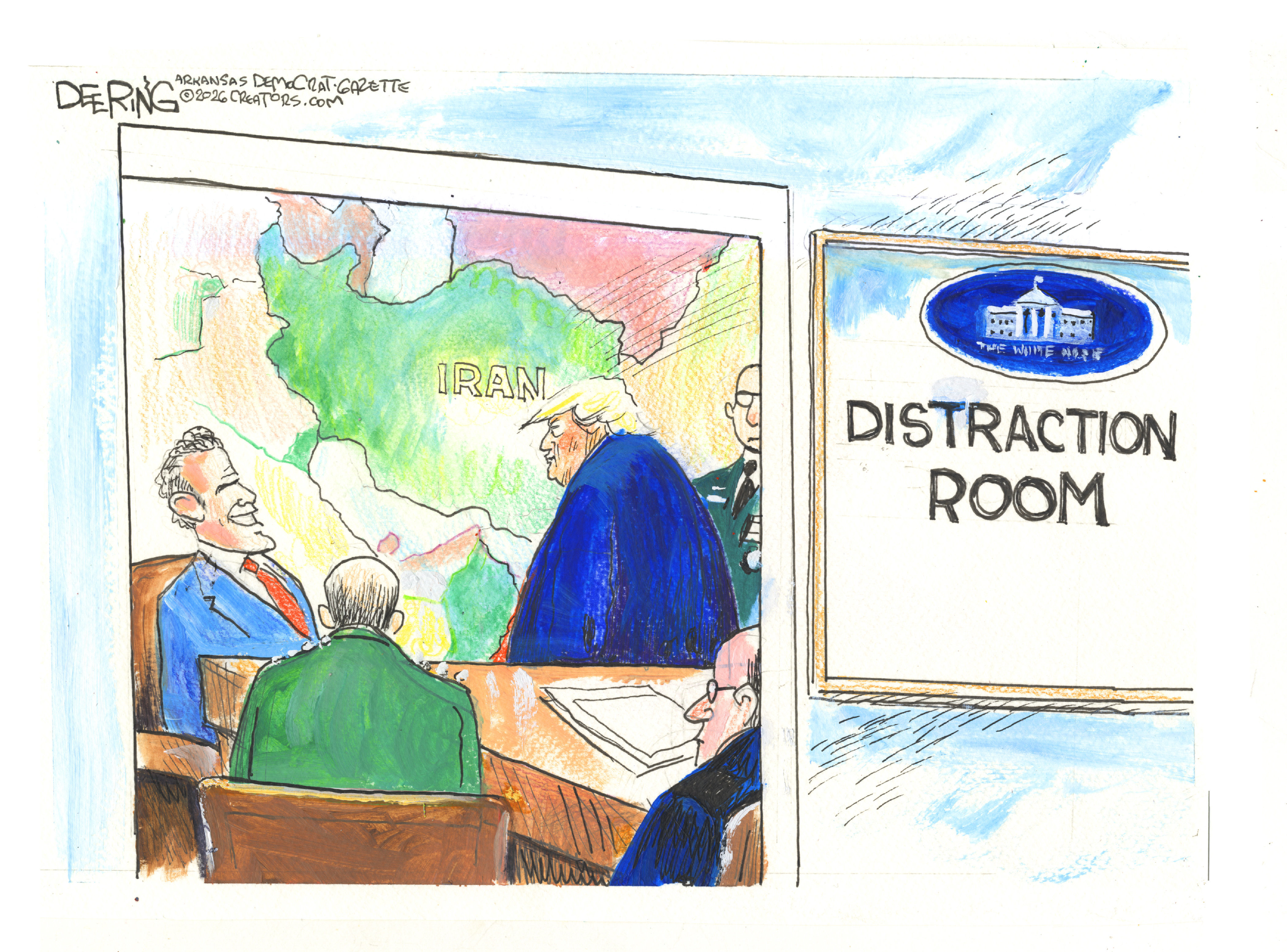 Political cartoons for February 21
Political cartoons for February 21Cartoons Saturday’s political cartoons include consequences, secrets, and more
-
 Crisis in Cuba: a ‘golden opportunity’ for Washington?
Crisis in Cuba: a ‘golden opportunity’ for Washington?Talking Point The Trump administration is applying the pressure, and with Latin America swinging to the right, Havana is becoming more ‘politically isolated’
-
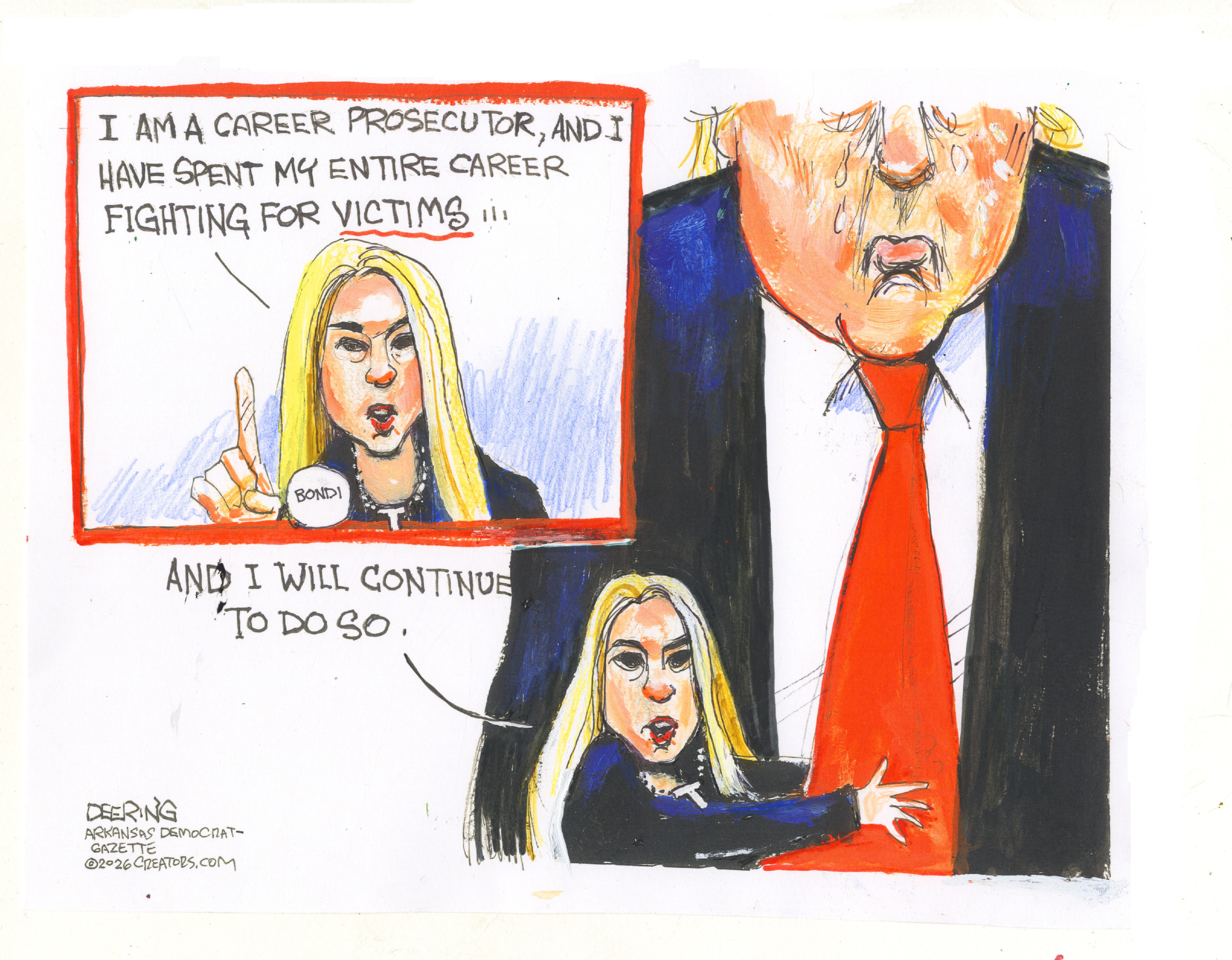 5 thoroughly redacted cartoons about Pam Bondi protecting predators
5 thoroughly redacted cartoons about Pam Bondi protecting predatorsCartoons Artists take on the real victim, types of protection, and more