Everything you need to know about the crisis in general practice
Patients are frustrated, medics are exhausted, and unions are enraged. What seems to be the problem?

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Why the frustration? Because many people are struggling to see their GPs. Patients complain they are being left waiting weeks for in-person consultations; a petition to “restart face-to-face appointments” attracted over half a million signatures.
After months of negative headlines, the Health Secretary Sajid Javid last month published a plan demanding improved patient access. He promised £250m in extra winter funding for GPs in England. However, doctors will be eligible for a share of the money only if they offered a certain proportion of face-to-face appointments; league tables will be published ranking them on this basis.
The plans went down well with campaigning newspapers – but were met with fury by GPs and unions, which said they scapegoated doctors and didn’t address underlying problems. The British Medical Association’s GPs committee unanimously voted to reject the measures, and is planning a ballot on possible strike action.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.

Are the problems pandemic-related?
To an extent, yes. Lockdowns have worsened patient backlogs. During the pandemic, GP appointments dropped sharply – in England, they fell by around 30% in April 2020 compared with the previous April. This created a backlog of patients awaiting planned hospital treatments, which GPs now have to manage, along with playing their part in the vaccine rollout and treating patients affected by Covid.
The pandemic also sharply accelerated a trend towards appointments being held virtually as opposed to in person. Pre-Covid, 80% of doctors’ appointments in England were face-to-face. But that figure fell to 47% in lockdown; it had only gone back up to 61% by September. In some areas, fewer than half of appointments have been held in person.
What’s wrong with virtual appointments?
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
Telephone consultations – along with video appointments – offer many advantages, particularly for initial triage. They save time for both doctors and patients, and allow the latter to avoid spending time in busy waiting rooms – crucial in a pandemic.
But most GPs would accept that there is often no substitute for face-to-face care. Virtual appointments exclude those without access to phones or internet, and make it harder for GPs to pick up on mental health issues or signs of abuse. But the main problem is the risk of missed diagnoses, in the absence of physical examination.
An official assessment by the Department of Health and Social Care and the Office for National Statistics into the “unintended consequences” of remote consultations found that more than 175,000 diagnoses of key conditions are estimated to have been missed last year alone. There was also a worrying 15% drop in the number of patients referred by GPs for urgent cancer check-ups last year.
So why aren’t GPs doing more?
They say they’re already doing everything they can. Family doctors are furious, complaining that they are being blamed for underlying problems in the system. Funding, they say, is inadequate: there has been a steady decline in the proportion of funding going to primary care, which deals with 90% of patient contacts, but gets only 10% of the budget.
And, worst of all, there’s a serious shortage of GPs. “This is a burnt-out workforce running on empty because of a massive mismatch between supply and demand,” declared the former health secretary Jeremy Hunt.
How bad is the shortage?
According to the Nuffield Trust, the UK had 0.6 GPs per 1,000 patients in 2018 – slightly fewer than the European average – though Scotland had a healthy 0.76, and England only 0.58. Since then, the BMA says the situation has become far worse: it estimates there are now just 0.45 fully qualified GPs per 1,000 patients in England – well below that of comparable wealthy nations – while the population is growing and ageing. And, despite a government promise in 2015 to hire 5,000 more GPs within five years, the number of full-time equivalent GPs actually fell by 4.5% between 2015 and March this year.
What’s behind that fall?
The BMA blames poor “workforce planning”: we have simply not, over the past decade, trained enough doctors. Admissions to UK medical schools have now risen to a high of 9,500 per year (up from 5,880 in 2015-16), but the trend will take time to reverse.
The UK also has trouble recruiting and retaining GPs. Fewer than 1% of GPs in England are under 30, compared to 23% who are over-55 and approaching retirement. According to the BMA, about half of existing GPs want to cut their hours, and 21% would like to leave the NHS altogether.

Are GPs overworked?
On some measures, certainly. The average number of patients per practice is 24% higher than in 2015. On the other hand, the average GP now works a three-day week. The authoritative National GP Worklife Survey shows that in 2019, GPs carried out just 6.6 half-day sessions a week – the equivalent of just over three days – the lowest on record. In 2010, it was 7.5 sessions. The BMA argues that this is thanks to a “vicious cycle” of overwork and GP shortages.
Are things likely to improve?
Probably not. Sajid Javid admitted this week that the Government is likely to miss its target of increasing the number of GPs in England by 6,000 by 2025, a key 2019 manifesto pledge. Javid is still insisting that patients must be offered in-person appointments unless there are “good clinical reasons”; the BMA accuses the Government of being “completely out of touch with the scale of the crisis on the ground”, ahead of what looks set to be a very difficult winter. Whatever happens on this issue, the underlying problems in GP recruitment and retention are unlikely to be solved any time soon.
-
 Switzerland could vote to cap its population
Switzerland could vote to cap its populationUnder the Radar Swiss People’s Party proposes referendum on radical anti-immigration measure to limit residents to 10 million
-
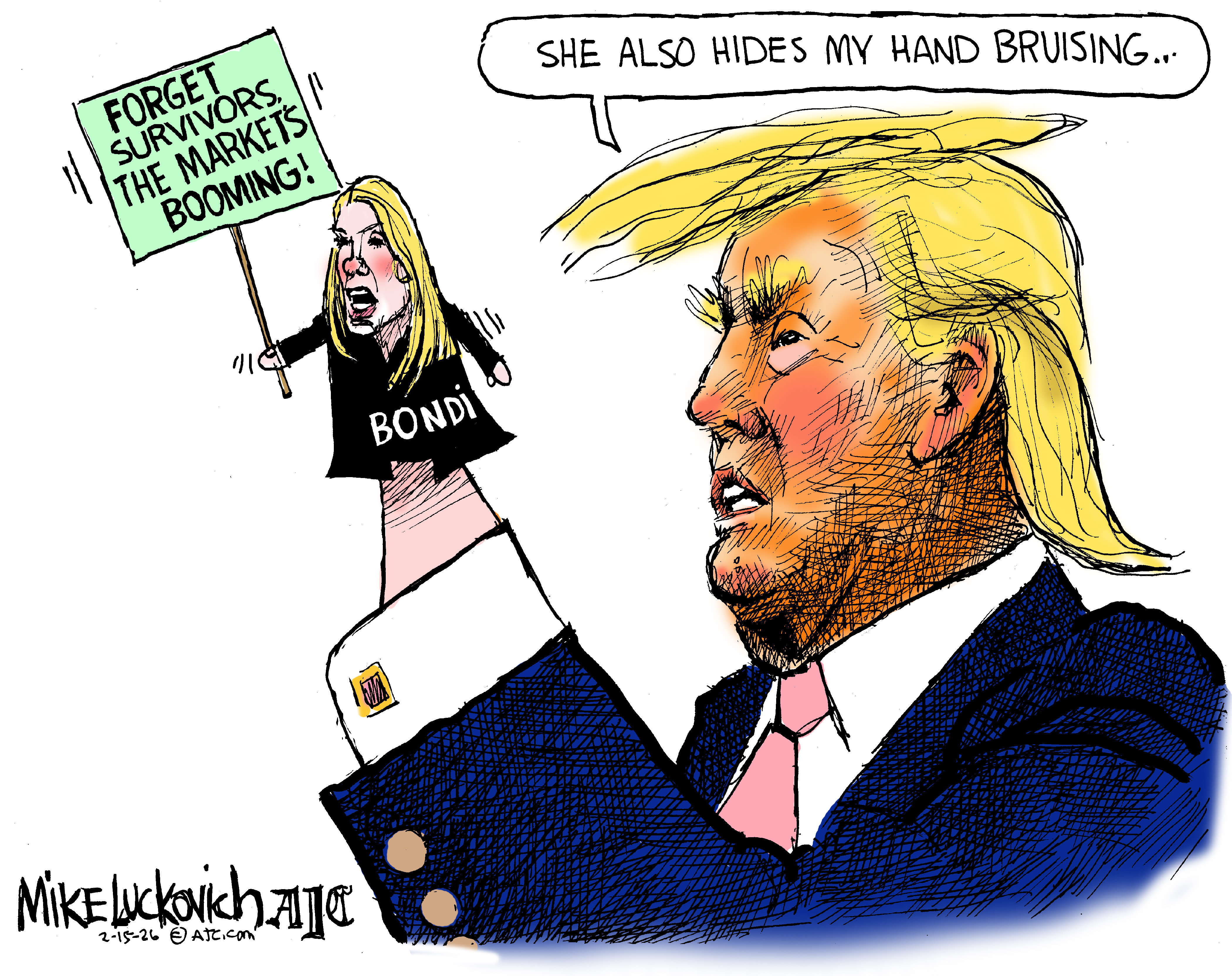 Political cartoons for February 15
Political cartoons for February 15Cartoons Sunday's political cartoons include political ventriloquism, Europe in the middle, and more
-
 The broken water companies failing England and Wales
The broken water companies failing England and WalesExplainer With rising bills, deteriorating river health and a lack of investment, regulators face an uphill battle to stabilise the industry
-
 Earring lost at sea returned to fisherman after 23 years
Earring lost at sea returned to fisherman after 23 yearsfeature Good news stories from the past seven days
-
 Bully XL dogs: should they be banned?
Bully XL dogs: should they be banned?Talking Point Goverment under pressure to prohibit breed blamed for series of fatal attacks
-
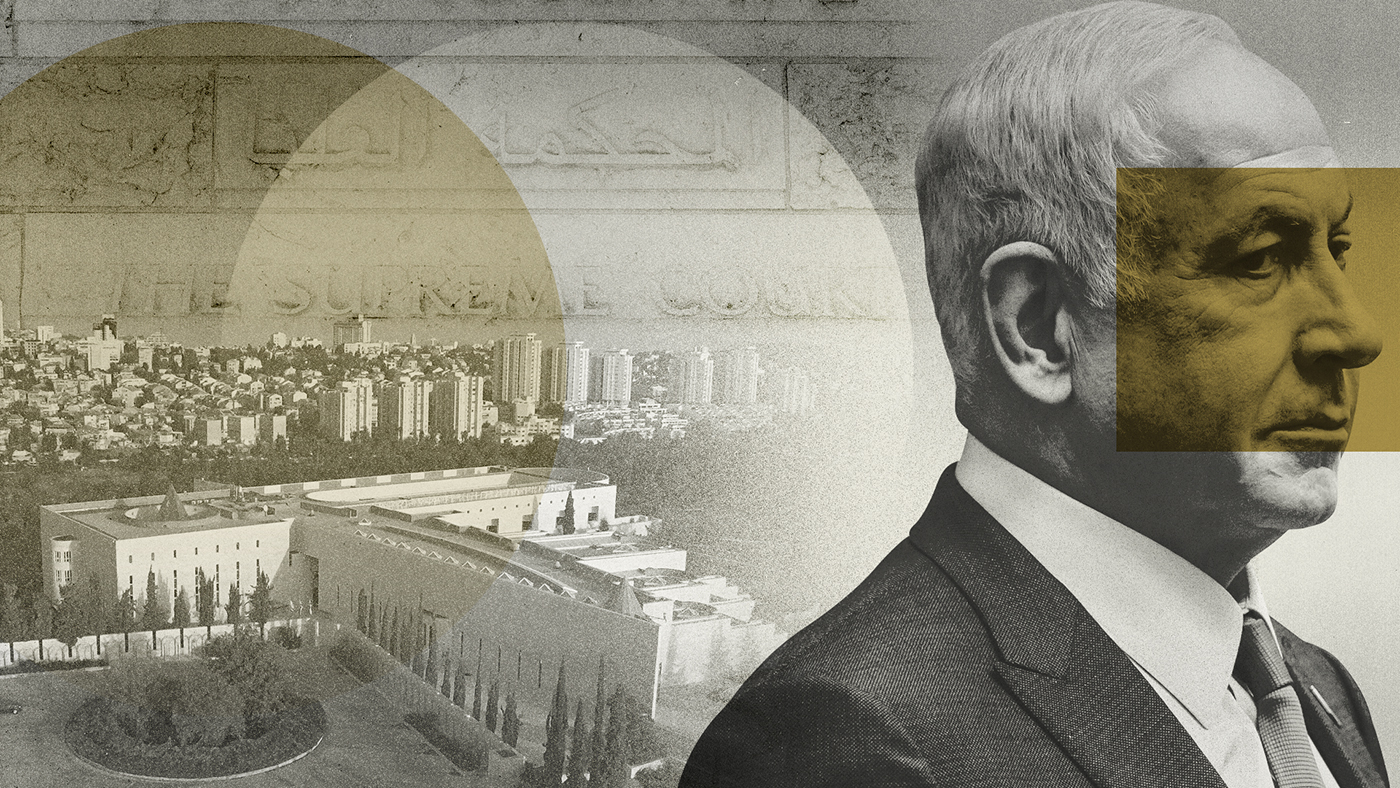 Netanyahu’s reforms: an existential threat to Israel?
Netanyahu’s reforms: an existential threat to Israel?feature The nation is divided over controversial move depriving Israel’s supreme court of the right to override government decisions
-
 Farmer plants 1.2m sunflowers as present for his wife
Farmer plants 1.2m sunflowers as present for his wifefeature Good news stories from the past seven days
-
 EU-Tunisia agreement: a ‘dangerous’ deal to curb migration?
EU-Tunisia agreement: a ‘dangerous’ deal to curb migration?feature Brussels has pledged to give €100m to Tunisia to crack down on people smuggling and strengthen its borders
-
 Manchester alleyway transformed into a plant-filled haven
Manchester alleyway transformed into a plant-filled havenfeature Good news stories from the past seven days
-
 China’s ‘sluggish’ economy: squeezing the middle classes
China’s ‘sluggish’ economy: squeezing the middle classesfeature Reports of the death of the Chinese economy may be greatly exaggerated say analysts
-
 Non-aligned no longer: Sweden embraces Nato
Non-aligned no longer: Sweden embraces Natofeature While Swedes believe it will make them safer Turkey’s grip over the alliance worries some