Deciding to die
A year after his mother's uncomfortable decline, a son asks: Should the terminally ill have control over when and how they die?

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful

If you're dying and don't care to wait around for death, you can always book your own appointment. One simple way to do this would be to stop eating and drinking; another would be to stop life-sustaining medicine or devices. Assuming you can decide on your own, both of these methods are good and kosher as far as the law goes. A third approach, however, ventures into a grayer area of legal and ethical terrain — quaffing a lethal cocktail. In the business of ending your life, the means matter a lot more than the final result.
These were three things my mother, Ann Krieger, was pondering when she reached the final leg of her terminal illness, a month before Mother's Day. After several years of fighting colon cancer, her doctor broke the news that the cancer had spread and the treatment was no longer working. There was no more they could do.
"You've got months, not weeks," he said.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
"What should I do?" she asked. "Should I end it now?"
"No," he said. "You don't want to do that."
Actually, my mother kind of did, but the doctor referred her to hospice and gave her information about palliative care, a mode of treatment that relieves the pain of patients with serious illnesses. But in my mother's case, the physical distress was less acute than the existential. Coming to terms with the fact that you're going to die is elusive. For some people, like her, an attempt to manage the logistics could make it seem more doable. She and my father had given this some thought and had very specific ideas about how they wanted their end-of-life matters handled.
(More from Narratively: Why the VFW is disappearing)
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
Six years earlier, horrified by what was taking place with Terri Schiavo in Florida, they sat my sister and me down to give us instructions. Should it ever come down to it, my parents told us, they wanted no artificial resuscitation, experimental procedures, machines, or IVs — none of that stuff. They just wanted us to make sure they would be allowed to die naturally. "The idea," my father explained to me recently, "is to be pain-free, comfortable and not go through a lot of unnecessary, costly and painful treatments which won't help anyway."
My mother had first-hand experience with this 21 years ago when her mom, my grandma Trixie, who was in perfect health at 85, was struck by a hit-and-run driver near her home in Queens. The doctors at New York Hospital said she had severe trauma in her brainstem and wouldn't wake up. She was hooked up to a ventilator.
Since there was no hope of her getting any better, my mother wanted to have the ventilator removed. She believed Trixie wouldn't have wanted to be left like that. But the doctors told her they couldn't do that. There had been a brain surgeon, my mother once mentioned, who had wanted to try out a procedure on her.
"Is it going to help her?" she asked him.
"No," he said, "it's not, but I'd like to do it for research."
She didn't give her approval, and the doctors wouldn't remove the ventilator. So my mother found someone high up in the hierarchy, a neurologist, who she was told might be sympathetic. She went to him and explained the situation. He was willing to give the order. Two days after the ventilator was disconnected, Grandma Trixie died.
Meanwhile, out in Forest Hills, my grandpa George Kaminsky, her husband, was on his own deathbed. Trixie had been out getting his medicine when she got hit crossing Queens Boulevard, grimly known as the "Boulevard of Death." A few weeks earlier she had been a sure bet to outlive him.
For months afterwards, George lay in bed, helpless and wasting away, with 24-hour nurses who washed and fed him and changed his diapers. He was lucid, and asked my mother and her sister to poison him. They told him they couldn't do that, but my aunt Nina pointed out that his medicine was probably keeping him alive. Ending his life merely by omission hadn't occurred to him.
"It was humane to put him out of his suffering but done through his choice," Aunt Nina told me recently. "He certainly acted on that information pretty quickly."
He died a few days later.
I believe that the power to make choices about how and when we die, when terminally ill, should be a basic human right. But there are various arguments against it. My favorite one says that it's not for mortals to make such decisions because we are in God's hands, however fumbling they may be. If God wants you to die in a certain manner, the logic seems to go, then that's because it's part of His plan. But what if God really doesn't care one way or the other? It would be quite an administrative headache, after all. Consider that across the globe, roughly 150,000 people die every day, at a rate of about 107 people per minute. A little human intervention could go a long way during that last bumpy stretch.
(More from Narratively: Freak show 101)
Many doctors, however, tend to think differently. Knowing this all too well, my mother had filed away the name of an organization she thought might offer some guidance when the time came.
The week she started hospice care, at the beginning of April 2011, my father, Melvin, contacted them. A few days later, they got a call from Judith Schwarz, the clinical coordinator of Compassion & Choices, who lived nearby on the Upper West Side. She came over and spent a few hours talking with my parents, explaining her organization's mission and discussing my mother's illness and the options available. "She was warm and it was personal," my father said. "She was a professional who is very skilled at dealing with situations like this."

Judith Schwarz, who is 68 years old, wears brown oval glasses and her hair short. She speaks with great precision, intensity and an uncanny command of the issues that comes from decades of being in the thick of it.
I paid her a visit this past spring. We sat in her spacious, sunlit living room, and as her Portuguese Water Dog slept on the floor we talked about my mother and end-of-life issues. The first thing Schwarz did was set me straight on the terminology when I asked about "assisted suicide." The term "suicide" has a lot of baggage, she explained, whether religious, legal or moral, so to call it "assisted suicide" or "euthanasia" is to miss a crucial distinction.
"We use the term 'aid in dying,'" Schwarz told me, "because it more accurately reflects the information and support we provide to terminally ill and suffering clients" — information about how patients might control the circumstances or timing of their death. She went on to say that the motivation for suicide, which often results from mental illness and depression, is another thing entirely. "We do not support suicide," she said, noting the difference between suicide and the "thoughtful and considered decisions" made by some terminally ill patients as a means to avoid further suffering.
(More from Narratively: Inside Manhattan's last peep shows)
When a patient in the Northeast contacts Compassion & Choices, he is referred to Schwarz, whose first order of business is to find out who the patient is and what his current medical situation entails. Then, Schwarz attempts to get a sense of what the patient is looking for. She tries to provide information to all callers, but to qualify for help, patients should be able to make their own decisions and be suffering, whether in a terminal stage of illness or not.
"There's a lot of misunderstanding about what we do," Schwarz said. "What we do is provide information about end-of-life choices to help patients make informed decisions that reflect their values and wishes. We don't provide the means. We don't administer. We don't encourage or coerce. We have no agenda other than to provide complete and accurate information about end-of-life options."
And in doing this, Schwarz's role is to help a patient navigate the end of his life so he can maintain some control over it, instead of leaving it to doctors who are trained not only to lessen suffering but also to keep him alive and death at bay.
One patient Schwarz consulted last spring needed help arranging to have his ventilator removed without suffering. Schwarz told me about what the process involved, which includes requesting support from palliative care clinicians who would see to it that the man did not experience pain, hunger for air, or anxiety.
Read the rest of the story at Narratively.
Narratively is an online magazine devoted to original, in-depth and untold stories. Each week, Narratively explores a different theme and publishes just one story a day. It was one of TIME's 50 Best Websites of 2013.
-
 El Paso airspace closure tied to FAA-Pentagon standoff
El Paso airspace closure tied to FAA-Pentagon standoffSpeed Read The closure in the Texas border city stemmed from disagreements between the Federal Aviation Administration and Pentagon officials over drone-related tests
-
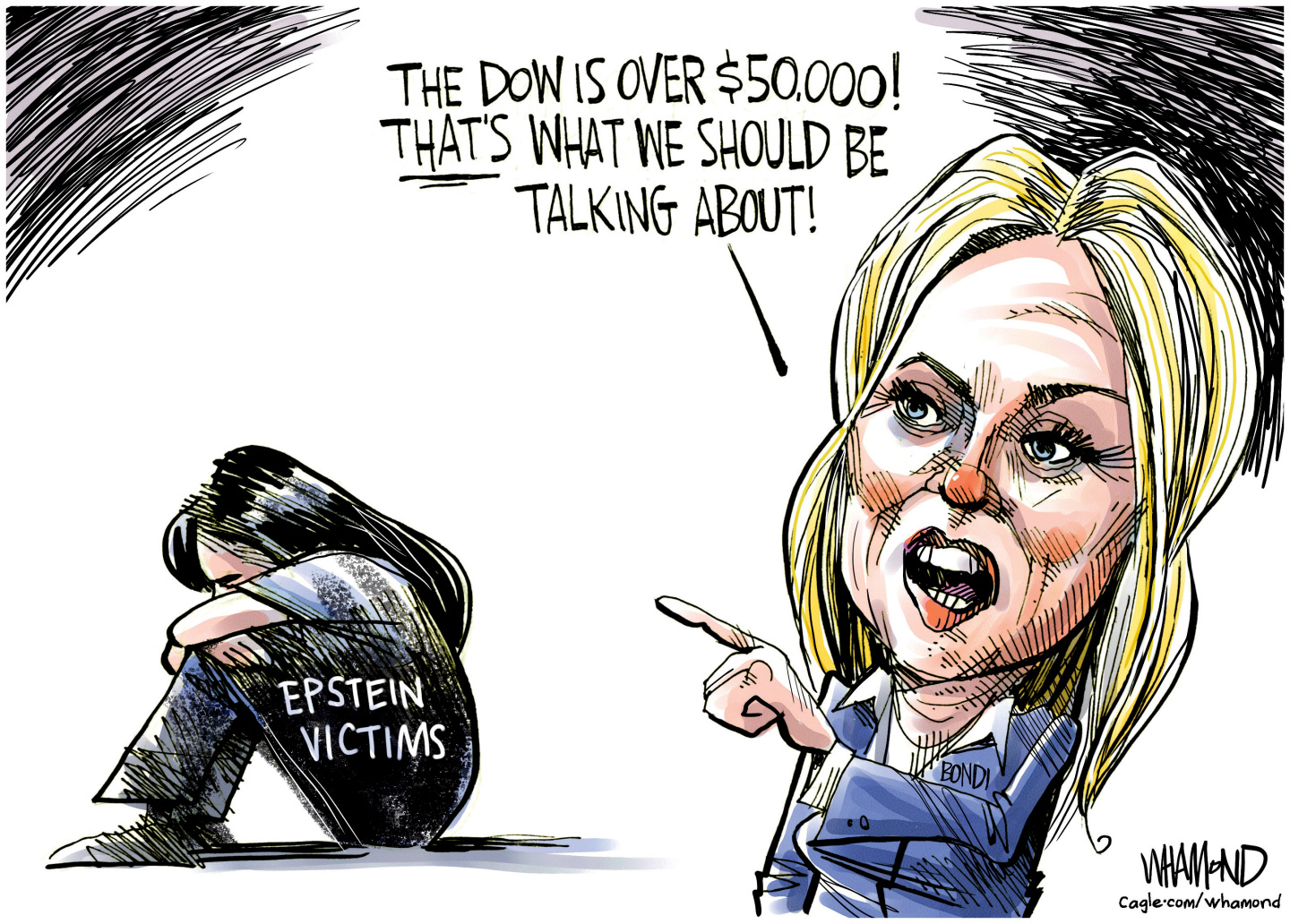 Political cartoons for February 12
Political cartoons for February 12Cartoons Thursday's political cartoons include a Pam Bondi performance, Ghislaine Maxwell on tour, and ICE detention facilities
-
 Arcadia: Tom Stoppard’s ‘masterpiece’ makes a ‘triumphant’ return
Arcadia: Tom Stoppard’s ‘masterpiece’ makes a ‘triumphant’ returnThe Week Recommends Carrie Cracknell’s revival at the Old Vic ‘grips like a thriller’