The ecosystem inside you
Your body harbors trillions of bacteria that have profound effects on your health, your weight, and even your mood
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Don't bacteria make people sick?
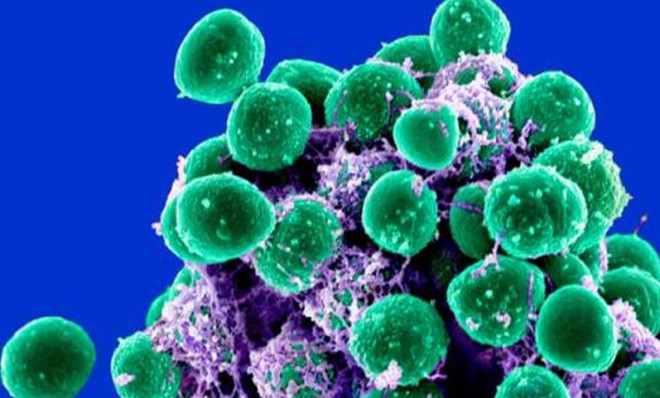
Many of them do, and antibiotics that kill them have saved countless lives. But over the past decade, researchers have discovered that the human body hosts 100 trillion mostly benign bacteria, which help digest food, program the immune system, prevent infection, and even influence mood and behavior. The bacteria living on and in us make up our "microbiome," an ecosystem that plays a role, scientists believe, in many conditions that genes and environmental factors alone can't explain, including obesity, autism, depression, asthma, and even cancer. The discovery of the microbiome, said Michael Fischbach, a bioengineer at the University of California, San Francisco, has been "very much like finding an organ we didn't know we had."
Where is the microbiome?
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
Bacteria thrive throughout our bodies — in our mouths and lungs, on our skin and teeth, and especially in our guts. The Human Microbiome Project, a government-supported effort to map our bacterial ecosystems, has discovered that people harbor 10 bacterial cells for every human cell. Every body hosts at least 10,000 different species of bacteria, contributing up to five pounds to body weight. "Half of your stool is not leftover food. It is microbial biomass," said project director Lita Proctor. Last year scientists presented evidence that everyone has one of three gut bacterial profiles, or "enterotypes," characterized by high levels of specific bacterial species. Some argue that enterotypes are as distinct as blood types, and that learning more about them will help us design better drugs and target them more effectively.
How do bacteria influence health?
Microbiome research is in its infancy, but there is already evidence that an imbalance of gut flora may cause gastrointestinal problems such as irritable bowel syndrome and Crohn's disease. Bacteria may also help calibrate our basal metabolism. When obese people undergo gastric bypass surgery to lose weight, scientists have observed, their gut bacteria become more like those harbored by thin people, contributing to weight loss. Microbes can even influence mental states by encouraging neurons in the intestines to signal the brain to alter hormone levels. Studies in mice have shown that changes in gut bacteria can relieve — or cause — depression and anxiety. It has also been shown that autistic children — who frequently suffer from gastrointestinal problems — often carry a type of gut bacteria that non-autistic children don't.
Why the difference in bacteria?
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
Some 80 percent of an individual's gut flora comes from his or her mother. A newborn exits the womb microbe-free, but is colonized by the mother's vaginal bacteria as it passes through the birth canal. Babies born via caesarean section, it turns out, enter life with an entirely different, and less diverse, collection of bacteria, which may help explain why they're at increased risk of asthma, obesity, and type-1 diabetes. Breast milk, unlike formula, also delivers maternal bacteria that help the immune system develop.
Can the microbiome change?
Yes, for good and for ill. Diet plays a major role in determining what bacteria people host. A recent study found that when certain gut bacteria feed on compounds in red meat or egg yolk, they produce an artery-hardening compound called TMAO. People who rarely eat red meat or egg yolks don't carry the same TMAO-producing bacteria and so can eat those foods occasionally without increasing their heart disease risk. Older people who live independently tend to have more diverse microbiomes than their frailer peers who live in nursing homes — maybe because of their different diets — but it's unclear whether a narrower microbiome causes declining health or is a consequence of it. Antibiotic use can also reduce gut flora. Researchers are still trying to determine what factors "could set the microbiota in a good direction versus a bad direction," said University of Colorado biochemist Rob Knight. "There are very few cases where cause and effect are known."
Can bacteria be used to treat illness?
In at least one case, they already are. C. difficile infections — caused by a bacterium that can take over the gut — cause severe diarrhea and kill 14,000 Americans per year. C. difficile is notoriously difficult to eradicate with antibiotics. But researchers have discovered that transplanting a healthy person's stool, via a tube inserted into the patient's stomach, cures the infection almost instantly by repopulating the patient's microbiome with healthy bacteria. Tellingly, C. difficile infections often begin after a person takes antibiotics to treat an unrelated condition. Some experts suggest that the widespread use of antibiotics, which kill good bacteria along with the harmful bacteria they target, could help explain the skyrocketing rates of asthma, obesity, and autism. "Whenever they are used, there is collateral damage, " said New York University microbiologist Martin J. Blaser. "And we are only now fully learning how severe that damage has been." Scientists are now trying to figure out what constitutes a healthy microbiome, in hopes they can treat health problems by tweaking the mix of a person's bacterial species. "The prospects here are endless," Blaser said. "This is the most exciting and important work of my lifetime."
The probiotics boom
Pills, drinks, and yogurts containing probiotics — live, beneficial bacteria — have become big business. In 2011, global sales of probiotics reached $28 billion and are expected to reach $42 billion in 2016. But experts remain skeptical of commercial claims, often unverified by clinical trial, that they bolster the immune system, improve digestion, and generally optimize our health. A review of probiotic research by scientists at Yale found that certain strains did appear to reduce diarrhea and alleviate irritable bowel syndrome, and other studies showed that they could shorten colds. But researchers still aren't sure which bacterial strains are helpful for which conditions, and how they interact with a given person's existing microbiome. "The science has been shoddy and flimsy," said bioengineer Michael Fischbach. Probiotics may well be the future of medicine, but they should "be more complicated and also more rigorously tested than today's probiotics," he says. "They'll be something that your doctor prescribes."