My alien heart
Amy Silverstein was a 24-year-old law student when a heart transplant saved her life. In a new book, she describes how daily meds, a ticking clock, and endless illnesses can wear down even a model patient.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Amy Silverstein was a 24-year-old law student when a heart transplant saved her life. In a new book, she describes how daily meds, a ticking clock, and endless illnesses can wear down even a model patient.
A heart biopsy is a kind of torture no person should have to endure, not even once. There is something unnatural about snipping vital tissue from a pulsing, life-giving organ. Even the healthiest of hearts is apt to buck and sputter in revolt as the pincer-grip end of the catheter moves in for the taking. Over the years, I’ve whiteknuckled my way through more than 60. I still get one when I have my annual checkup. Patients are awake. They may cry out when they feel pieces of their hearts being snatched from them this way. They are likely to perceive the maneuver as a nasty yank, not the little tug that biopsy doctors promise. It’s not just one, either. Sometimes it has taken my doctor 30 tries. The day following my first biopsy, a Dr. Bradley stood at the foot of my hospital bed. “You have, or you had, at some time, a virus in your heart,” he said. “There is some scarring. The damage may be on the mend.” He put me on some cardiac medications. “Your heart needs to rest and recover—and repair itself, I hope.” Several months later, my heart was still acting up. A fluttering in my chest tugged constantly at my awareness. But Scott, my boyfriend, was graduating from Penn’s law school, and I had come down to Philadelphia from New York on my usual Friday-night train for the ceremony. He began listing restaurant options: Italian, Japanese, maybe Indian. I hid that I’d been fighting nausea for two weeks. I told him Japanese sounded terrific. Toward the end of the meal, my heart began skipping beats, then pounding wildly. I began a sentence—and a heartbeat stopped me. I knew right away this one was different. This was ventricular fibrillation, V-fib, the killer. “Scotty, I don’t feel right,” I said. It was obvious to the ER doctors that there was no time for a slow drip of antiarrhythmia drugs; they needed to save my life. I would need to be defibrillated immediately. I saw the paddles coming toward my chest. The sound of my own words echoed back at me as if they were coming from someone else: “Don’t let me die.” “You’re a very sick girl, Amy,” said Dr. Bradley the next morning. That label would settle in place like cement. “Sick girl” held more meaning for me than “cardiomyopathy” ever could. The words were to creep into every thought I would ever have about myself: I am a lawyer and a mother—but I am a sick girl; it’s the 10th anniversary of my heart transplant— but I am a sick girl; Scott is the love of my life—but I am a sick girl. Back in New York, I met with a new cardiologist, Dr. Ganz. “I don’t think any medicine is going to work,” he told me. “You need to have a heart transplant.” “I won’t do it.” “There really isn’t any option. We can get the paperwork going. You’ll be on the list in a few days.” “I said I won’t do it!” I yelled. My father was weeping at my bedside. I felt desperate to escape his anguish. “Okay,” I said. I was the luckiest patient at Columbia Presbyterian that June in 1988—young and desperately sick, making me No. 1 on the waiting list for the New York area. I turned 25 in the hospital. I got engaged. Scott knelt at my bedside. “I was wondering,” he said. “Will you marry me?” I shouted out, “Yes!” A new heart was transplanted into my body on June 24. “Please don’t let me die,” I said to Dr. Solomon, the transplant surgeon. He was well used to not letting people die. He knew that by the end of my surgery he would have performed “just another everyday miracle,” as heart transplant surgeons say when they emerge from the operating room. He was pleased to report to the waiting-room group that my donated heart had burst into robust, vigorous beats from the moment the heart-lung machine was switched off. It just flew on its own. My new heart had a 10-year life expectancy, and I was warned how difficult the first year would be, living with high levels of immunosuppressant drugs and an ever present risk of my body’s rejecting my new heart. But no doctor had explained to me just how I was supposed to live out my ticking clock. There was something else no one spoke of before I got out of the hospital: Transplanted hearts do not feel natural most of the time. They cannot beat normally, because they have been cut off forever from the central nervous system. When they took out my heart, and took out my donor’s heart, all the nerves were severed. It’s not possible to reattach the bloody tangle of dangling nerve fibers. Without nerve connections to instruct the heart to speed up, slow down, or maintain the status quo, a transplanted heart will rely on the flow of adrenaline in the bloodstream. When excitement or fear hits, the typical transplant heart will flounder until a rush of adrenaline—often in overabundance—arrives. This constant dependence on adrenaline causes a very fast resting pulse—usually around 100 beats per minute—that can be set off into a racing gallop by additional adrenaline dumped into the bloodstream. But there’s a delay. I tried to explain it to a friend. “If you come up behind me and yell boo! I’ll know you did it, but my heart won’t, not at first. A few minutes later, the adrenaline kicks in, and my heart will start beating like wild.” When the extra slug of adrenaline hits my heart, I feel like I’m going to die on the spot, a terrifying sense that I’m on the edge of ventricular fibrillation. The baffled pump beneath my breastbone reminds me over and over that when it is asked to rise to an occasion, it has no idea what in hell to do. I’m caught in a body that thinks it’s just now had a boo! moment that’s come and gone. My heart Lucky girl: The author at her 1990 law school graduation should have returned to its resting state; instead, it’s riding high and wild on a tidal wave of adrenaline. Scott and I were married at 7 o’clock the evening of June 24, 1989, exactly one year after my transplant. I drifted down the aisle. One year ago, at this same time, I was on an operating table attached to a heart-lung machine. I had to break away from the party at the stroke of 10 to squirt a syringe of cyclosporine into my mouth. A dose was necessary every 12 hours, and no playing around with the timing. Squirt: a shot of nauseating bitterness. Slurp: a swig of apple juice stashed with the cyclosporine. Done. A quick dash through the gilded hallways, and I would be back at my grand wedding, looking no worse but feeling quite different. Cyclosporine was my prescribed poison. In just a few minutes, nausea would rock my limbs with land-borne seasickness. My hands would shake. The shaking would become intense, driving me off the dance floor. There would be a headache, the kind that tries to twist my face into a wince. I would fight my way through the side effects. I would not reveal them. From the moment I introduced my body to a whopping dose of immunosuppressants, I could feel it recoil from what the chemicals were trying to do. Every day, twice a day, I felt this war coursing through me and was sickened, not just by the physical side effects but also by the disturbing thought that I had to poison the most health-giving system in my body in order to stay alive. What is 10 years to a 25-year-old woman? I had not been robbed of my youthful mindset. I was still just a woman for whom 10 years could be perceived as a good long time. It was practically a lifetime. But time passed quickly. At first, I counted in post-transplant years: one year after, two years after, three years after. Somewhere around seven, the count would become more focused on my future. Year eight was “two years left before I’m supposed to die,” and year nine was the oneyear warning. At year 10, the counting system would shift to borrowed time. The years would become eggshells that I would walk on with diminishing confidence: I should have been dead one year ago; I should have been dead two years ago. ... Ten years would no longer be a gift. It would be a curse. I felt more and more vulnerable. My likelihood of survival would decrease as time went by. There is no point at which, statistically speaking, a heart-transplant patient is on safer ground, because from the moment a donor heart begins to beat in a foreign chest, the immune system begins to destroy it. The sound of time passing became unbearably loud, but no one around me heard it. “You always make the best salad!” they’d rave. I’d been sick when I made that salad, so weak I had to sit down at the kitchen table three times before I got around to chopping the tomatoes. Hospitalizations, clinic visits, heart biopsies, illnesses, infections—everyone preferred to pay attention to other things. A surgery no longer warranted a phone call from a friend. Why bother? Amy has them all the time. A 10-hour emergency-room visit, complete with medical errors and a hospital admission at 3 a.m., was just another big yawn to those who looked on. It was just something Amy did. I landed in a therapist’s office. “Suffering is suffering,” Dr. Fisher told me. This was supposed to make me feel better? Two years ago, a Dr. Allen pressed two fingers far up into my armpit. When his fingers reached the lymph node, his eyes closed tight as if something had just caused him great pain. “Yeah, yeah, I feel it,” he said. Here it was, after 17 years, I thought. Post-transplant lymphoma. Cancer. I couldn’t find my breath. “Get dressed,” he barked. “Get on the phone. Call your transplant cardiologist. You need to biopsy this lump—now. You don’t want to waste one minute, believe me.” I was frozen in place. To start down this road would mean breaking a promise I’d made to myself soon after my transplant: I would fight through the little illnesses, and I’d even do the bigger ones if I had to, but never again would I fight the killers that were going to get me no matter what I did. I didn’t yet know that the whole crisis would prove to be only another scare when Dr. Allen came back to the exam room. “Did you call?” he asked. I stared at the floor, ashamed. “I can’t. I mean, I won’t. I can’t do cancer, Dr. Allen.” “You can do this, easy,” he said. “Don’t be ridiculous.” Dr. Allen was keeping other patients waiting. But he held my hands tight until he could tell that it was okay to let go. From Sick Girl by Amy Silverstein. Reprinted with the permission of the publisher, Grove/ Atlantic, Inc. ©2007 by Amy Silverstein. Adapted from an excerpt that originally appeared in U.S. News & World Report.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
-
 Tourangelle-style pork with prunes recipe
Tourangelle-style pork with prunes recipeThe Week Recommends This traditional, rustic dish is a French classic
-
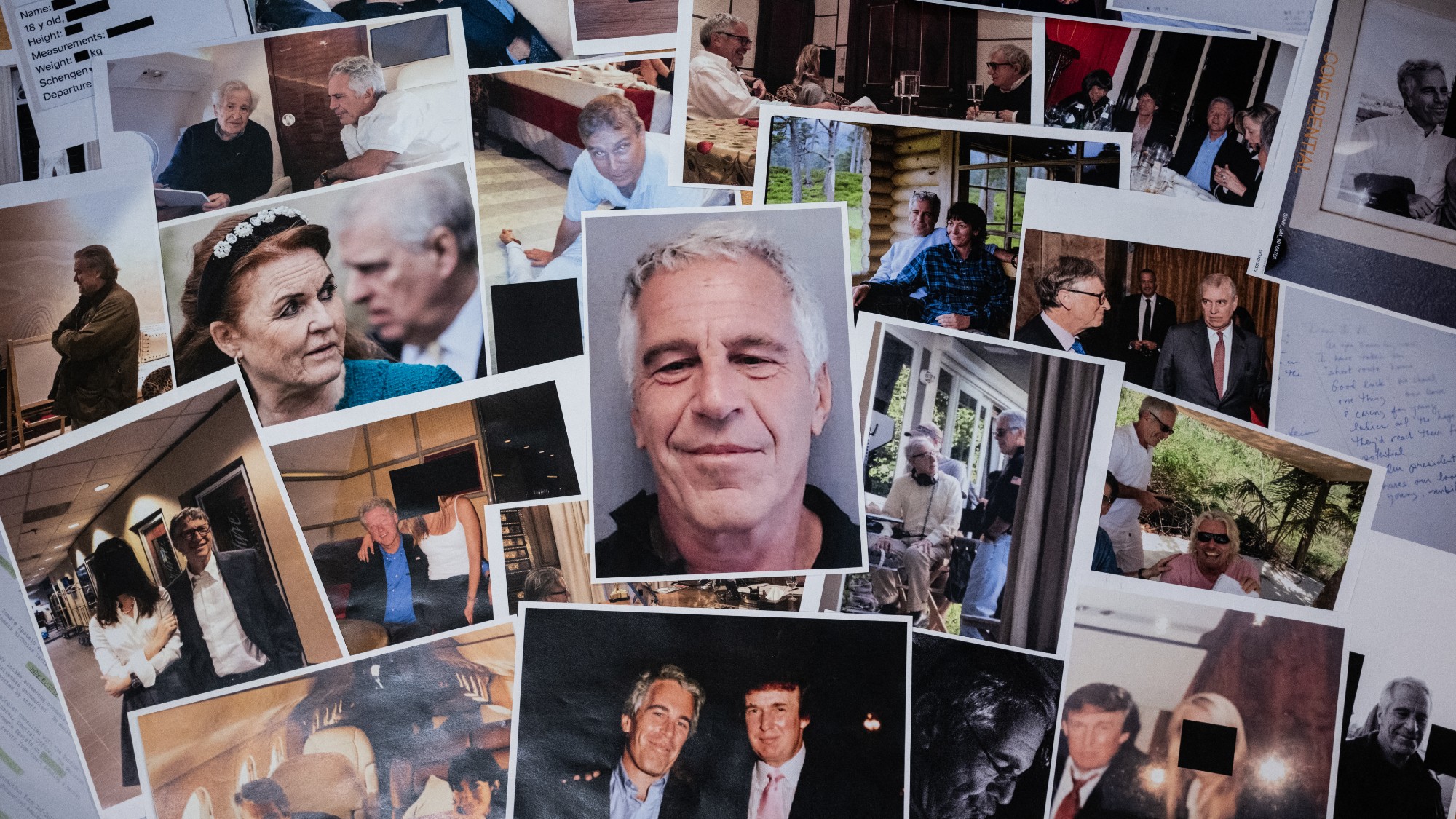 The Epstein files: glimpses of a deeply disturbing world
The Epstein files: glimpses of a deeply disturbing worldIn the Spotlight Trove of released documents paint a picture of depravity and privilege in which men hold the cards, and women are powerless or peripheral
-
 Jeff Bezos: cutting the legs off The Washington Post
Jeff Bezos: cutting the legs off The Washington PostIn the Spotlight A stalwart of American journalism is a shadow of itself after swingeing cuts by its billionaire owner