The promise and peril of CVS buying Aetna
Will the merger result in a big friendly giant — or a market-devouring monster?


A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
A few days ago, the pharmacy retailer CVS announced it would purchase health insurer Aetna for a cool $69 billion. The deal is one of the largest of 2017, and would create a health-care behemoth. Supporters of the deal — including, needless to say, the CEOs of both companies — argue it will deliver efficiencies, better service, and lower prices for customers. Critics worry it will drive even more consolidation in a health industry already dominated by giants, and leave everyone else worse off in the long term.
As it turns out, both arguments might be true.
First, the lay of the land: With almost 10,000 drugstores, CVS is one of the biggest players in the retail pharmacy market. But some of its $177 billion in revenues last year also came from its mail-order drug operation and sales of specialty medicines, along with the over 1,000 walk-in clinics it operates.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
Meanwhile, Aetna is a health insurer that boasts 22 million customers and over $63 billion in revenue.
CVS has also been serving as Aetna's pharmacy-benefit manager (PBM) since 2010. A PBM is a kind of middle man between drug manufacturers and health insurance providers, and negotiates bulk discounts on drugs for the latter. With almost one quarter of all prescription drug sales under its command, CVS accounts for an equivalent portion of the PBM industry. Add in Express Scripts and UnitedHealth (OptumRx), and those three PBMs control almost three-fourths of the market.
This is where the case that the merger could benefit consumers begins. PBMs were supposed to help lower drug prices. But like a lot of middle men in health care, they arguably jack prices up and pocket the surplus.
With the CVS-Aetna merger, the job of negotiating drug prices and providing insurance will be brought under the same roof instead. And since OptumRx already exists under the auspices of the insurer UnitedHealth, we could be seeing "the beginning of the end of the standalone pharmacy benefits manager business," as Craig Garthwaite, a Northwestern University health economist, put it to the The New York Times.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
But it doesn't stop there. Because it would control drug sales, medical care provision through its walk-in clinics, and insurance coverage to boot, the CVS-Aetna merger could create a chain of local "one-stop shops" for health care. Customers wouldn't just come in for medicine, but to deal with everything from a sore throat to more chronic issues like diabetes or obesity. Having both insurance and the care provision business under one roof could also allow for better use and dissemination of patient information, resulting in smarter and more efficient coordinated care, and thus (hopefully) lower insurance premiums. Since CVS will also retain its retail chains for other products like groceries and beauty supplies, it will also have an incentive to encourage patients to come into the physical locations more often — say, by pushing more regular checkups and preventative care.
One of the longest-running problems in American health insurance is how to get coverage providers to stop competing over who can best game the risk pools, and start competing on who can deliver the best care to patients. So the optimistic case for the CVS-Aetna merger is that it pushes things in that direction.
"We think of it as creating a new front door to health care in America," CVS Health CEO Larry J. Merlo said. "We know we can make health care more affordable and less expensive."
Whether it will actually work out that way is another matter.
Critics point out that UnitedHealth's ownership of OptumRx hasn't succeeded in bringing down prices. On top of that, CVS already has about a thousand walk-in clinics that haven't produced notable savings either, Carnegie Mellon health economist Martin Gaynor noted. And even by themselves, CVS and Aetna already have considerable scale with which to improve quality and prices for patients if they wanted to.
An alternative explanation for the CVS-Aetna merger is that, rather than a pro-active effort to improve their product, the deal is a defensive move to preserve market share in a health industry that's already rapidly consolidating. As the Times reports: "Insurers are buying or partnering with health-care providers. Health systems are offering insurance. Hospitals are employing physicians." Amazon also acquired pharmaceutical licenses in 12 states. They weren't for distributing drugs; they were for distributing medical equipment. But the event still had everyone freaking out that Amazon and its market-eating business model were coming for prescription drugs.
Insurers have also been trying to combine with other insurers as well, but the government has become at least somewhat skeptical of mergers among competitors in the same line of business: It previously squashed Aetna's attempt to combine with Humana, for instance. The CVS-Aetna merger would be an example of "vertical integration" — a combination between two businesses at different points in the supply chain — and thus ostensibly less offensive to antitrust enforcement. But the government could start cracking down on that too.
In the short run, one way to deal with a behemoth in a market is to create another giant through another merger. But that's an unsustainable solution: Eventually, you run out of companies to combine, and wind up under an oligopoly.
The CVS-Aetna combo could provide lower prices and premiums at its one-stop shops initially. But it has no reason to provide those benefits to customers on its insurance plan who need to go to non-CVS-Aetna providers. And eventually, its one-stop shops could become the only shops in many communities. Then it has no incentive to pass along savings to customers at all.
At any rate, the deal will close in the second half of 2018, assuming regulators allow it. So we'll see soon enough.
Editor's note: An earlier version of this article misstated details about Amazon's purchases of pharmaceutical licenses. It has since been corrected. We regret the error.
Jeff Spross was the economics and business correspondent at TheWeek.com. He was previously a reporter at ThinkProgress.
-
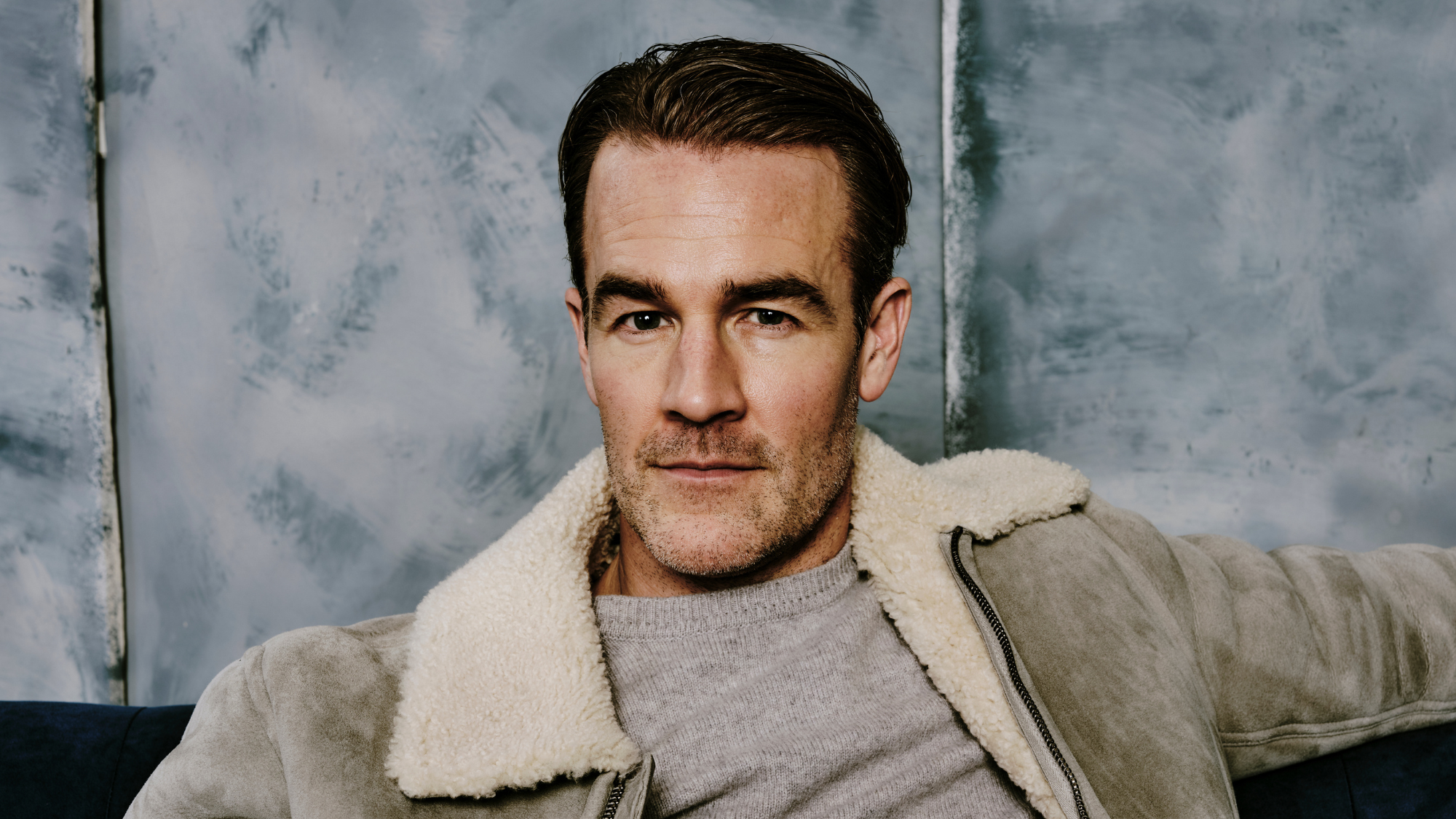 James Van Der Beek obituary: fresh-faced Dawson’s Creek star
James Van Der Beek obituary: fresh-faced Dawson’s Creek starIn The Spotlight Van Der Beek fronted one of the most successful teen dramas of the 90s – but his Dawson fame proved a double-edged sword
-
 Is Andrew’s arrest the end for the monarchy?
Is Andrew’s arrest the end for the monarchy?Today's Big Question The King has distanced the Royal Family from his disgraced brother but a ‘fit of revolutionary disgust’ could still wipe them out
-
 Quiz of The Week: 14 – 20 February
Quiz of The Week: 14 – 20 FebruaryQuiz Have you been paying attention to The Week’s news?
-
 The pros and cons of noncompete agreements
The pros and cons of noncompete agreementsThe Explainer The FTC wants to ban companies from binding their employees with noncompete agreements. Who would this benefit, and who would it hurt?
-
 What experts are saying about the economy's surprise contraction
What experts are saying about the economy's surprise contractionThe Explainer The sharpest opinions on the debate from around the web
-
 The death of cities was greatly exaggerated
The death of cities was greatly exaggeratedThe Explainer Why the pandemic predictions about urban flight were wrong
-
 The housing crisis is here
The housing crisis is hereThe Explainer As the pandemic takes its toll, renters face eviction even as buyers are bidding higher
-
 How to be an ally to marginalized coworkers
How to be an ally to marginalized coworkersThe Explainer Show up for your colleagues by showing that you see them and their struggles
-
 What the stock market knows
What the stock market knowsThe Explainer Publicly traded companies are going to wallop small businesses
-
 Can the government save small businesses?
Can the government save small businesses?The Explainer Many are fighting for a fair share of the coronavirus rescue package
-
 How the oil crash could turn into a much bigger economic shock
How the oil crash could turn into a much bigger economic shockThe Explainer This could be a huge problem for the entire economy
