Why people can't access dementia 'wonder' drugs
New immunotherapy drugs offer some hope in the fight against Alzheimer's disease but they're too pricey for the NHS

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
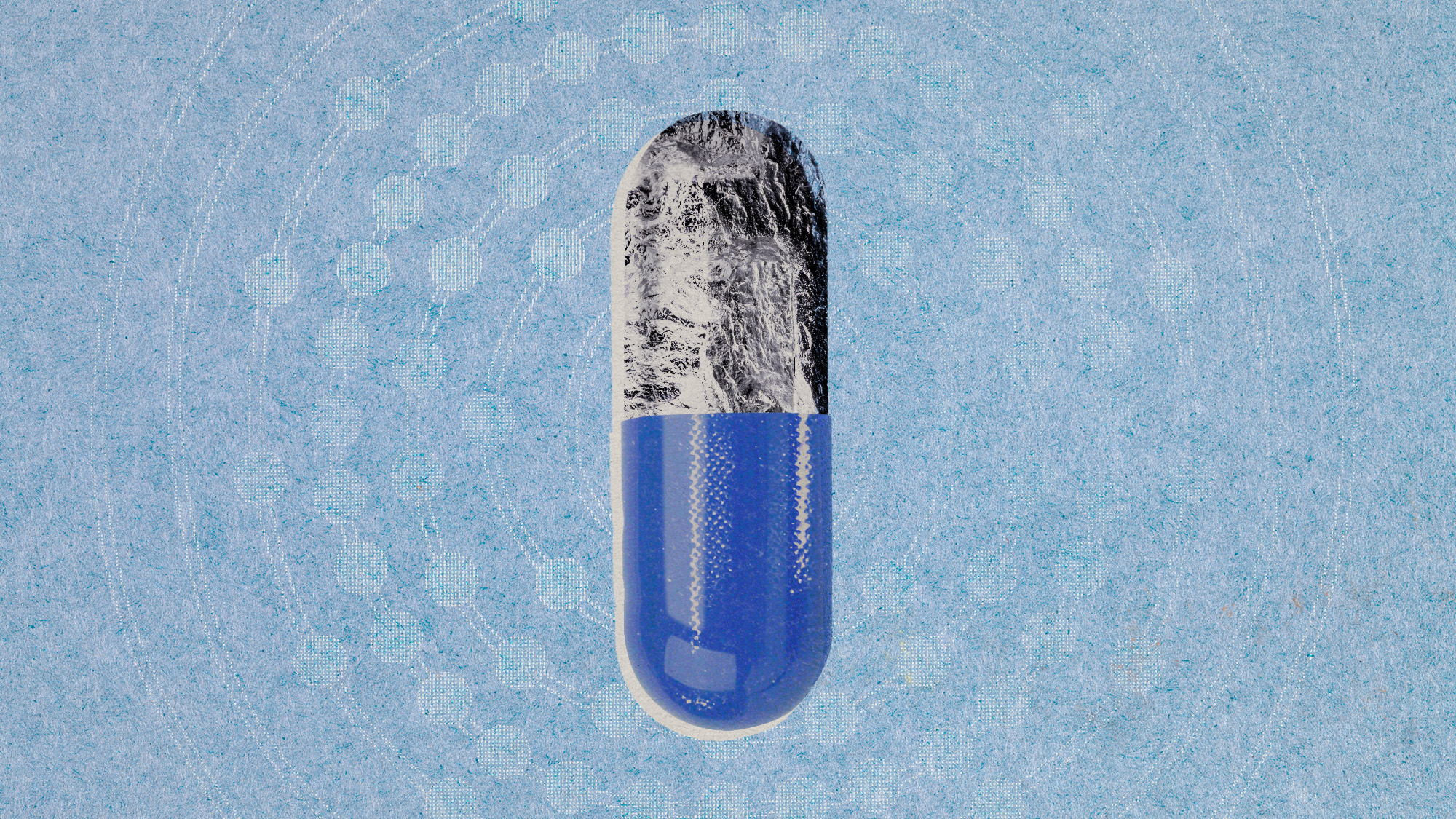
The NHS will not be rolling out two new drugs that have been hailed as landmark treatments for Alzheimer's disease. Lecanemab and donanemab are the first drugs to slow the progress of the disease but the independent body that decides which medicines should be available on the NHS has concluded that neither has benefits that justify their high cost.
"Neither drug can be recommended," said the National Institute for Health and Care Excellence in its final assessment last week, because the "overall costs of purchasing and administering the drugs remain high and the benefits too small". Both lecanemab and donanemab have been approved as medicines in UK, so will be available privately.
How do the new drugs work?
Both lecanemab and donanemab are monoclonal antibodies, created in a lab to target amyloid beta proteins, which accumulate in clumps, or plaques, in the brain of people with Alzheimer's disease. Delivered through an IV infusion, the drugs bind to the amyloid proteins and then attract the body's own antibodies to attack and break them down. The two drugs operate similarly but lecanemab targets the amyloid proteins as they begin to clump together, while donanemab binds to the proteins once they've clumped together to form larger plaques.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
How effective are the new drugs?
Neither drug reverses or stops the disease but it's thought they could potentially delay the cognitive decline of patients in the early stages of Alzheimer's by between four and seven months. Trials have shown that lecanemab can slow decline in memory and thinking by 27%, and donanemab by 35%.
But there are some caveats. The benefits seem to be better for men than women and, as the trial participants were generally young, white and with no other health conditions, it's likely that real-world effectiveness on older, frailer, more diverse Alzheimer's patients might be less impressive. By selecting participants the way they did, the researchers "were giving the drugs the best possible chance to show an effect", Seb Walsh, a doctoral fellow specialising in dementia and public health at Cambridge University told Unherd. And yet, even so their impact was "so small, it probably wouldn't be noticeable to a doctor".
"I understand the benefits of the drug are modest and that is as much as we can expect from any of these new Alzheimer's drugs at this point," Peter Almond, a clinical trial participant, told The i Paper last year. "But if it has been stopping my condition developing into Alzheimer's, then it has had a significant impact on my life."
Why are the drugs so expensive?
It's down both to the cost of the drugs themselves, and the way they need to be administered.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
Before starting treatment, an Alzheimer's diagnosis must be confirmed via an expensive positron emission tomography scan or a lumbar puncture. Then each patient needs an IV infusion every two weeks, along with regular brain scans and check-ups to monitor effectiveness and potential side effects (which are known to include potentially fatal brain swelling and brain bleeds or haemorrhages). These processes effectively double the cost, from roughly £20,000 to £25,000 per patient per year for the medicine itself to at least £50,000.
Should the NHS fund the drugs?
There are roughly 70,000 people in the UK with mild Alzheimer's disease who could be eligible for the new drugs, if they were to be funded by the NHS. The cost to the health service of such a rollout was estimated, in a 2024 NHS briefing paper, at between £500 million and £1 billion a year.
"The substantial resources the NHS would need to commit" mean that "if they were approved, they could displace other essential treatments and services", said the National Institute for Health and Care Excellence.
Those frustrated by the decision see this not only as a disappointment for those affected by Alzheimer's disease but also as a setback in research into an eventual cure. Others contend that the price-per-patient, not to mention the social benefit of people remaining independent for longer, pales in comparison to the vast expense of supporting people in the latter stages of Alzheimer's disease and in care homes.
But all the focus on so-called "wonder drugs", Tom Dening, director of the Centre for Dementia at the University of Nottingham, told The i Paper, is "a bit of a distraction from the main issue – which is to help people live the best lives they can with the diagnosis".
-
 ‘Poor time management isn’t just an inconvenience’
‘Poor time management isn’t just an inconvenience’Instant Opinion Opinion, comment and editorials of the day
-
 Bad Bunny’s Super Bowl: A win for unity
Bad Bunny’s Super Bowl: A win for unityFeature The global superstar's halftime show was a celebration for everyone to enjoy
-
 Book reviews: ‘Bonfire of the Murdochs’ and ‘The Typewriter and the Guillotine’
Book reviews: ‘Bonfire of the Murdochs’ and ‘The Typewriter and the Guillotine’Feature New insights into the Murdoch family’s turmoil and a renowned journalist’s time in pre-World War II Paris
-
 Scientists are worried about amoebas
Scientists are worried about amoebasUnder the radar Small and very mighty
-
 Metal-based compounds may be the future of antibiotics
Metal-based compounds may be the future of antibioticsUnder the radar Robots can help develop them
-
 A real head scratcher: how scabies returned to the UK
A real head scratcher: how scabies returned to the UKThe Explainer The ‘Victorian-era’ condition is on the rise in the UK, and experts aren’t sure why
-
 How dangerous is the ‘K’ strain super-flu?
How dangerous is the ‘K’ strain super-flu?The Explainer Surge in cases of new variant H3N2 flu in UK and around the world
-
 Choline: the ‘under-appreciated’ nutrient
Choline: the ‘under-appreciated’ nutrientThe Explainer Studies link choline levels to accelerated ageing, anxiety, memory function and more
-
 RFK Jr. sets his sights on linking antidepressants to mass violence
RFK Jr. sets his sights on linking antidepressants to mass violenceThe Explainer The health secretary’s crusade to Make America Healthy Again has vital mental health medications on the agenda
-
 The ‘menopause gold rush’
The ‘menopause gold rush’Under the Radar Women vulnerable to misinformation and marketing of ‘unregulated’ products
-
 Peanut allergies have plummeted in children
Peanut allergies have plummeted in childrenUnder the radar Early introduction could be an effective prevention method