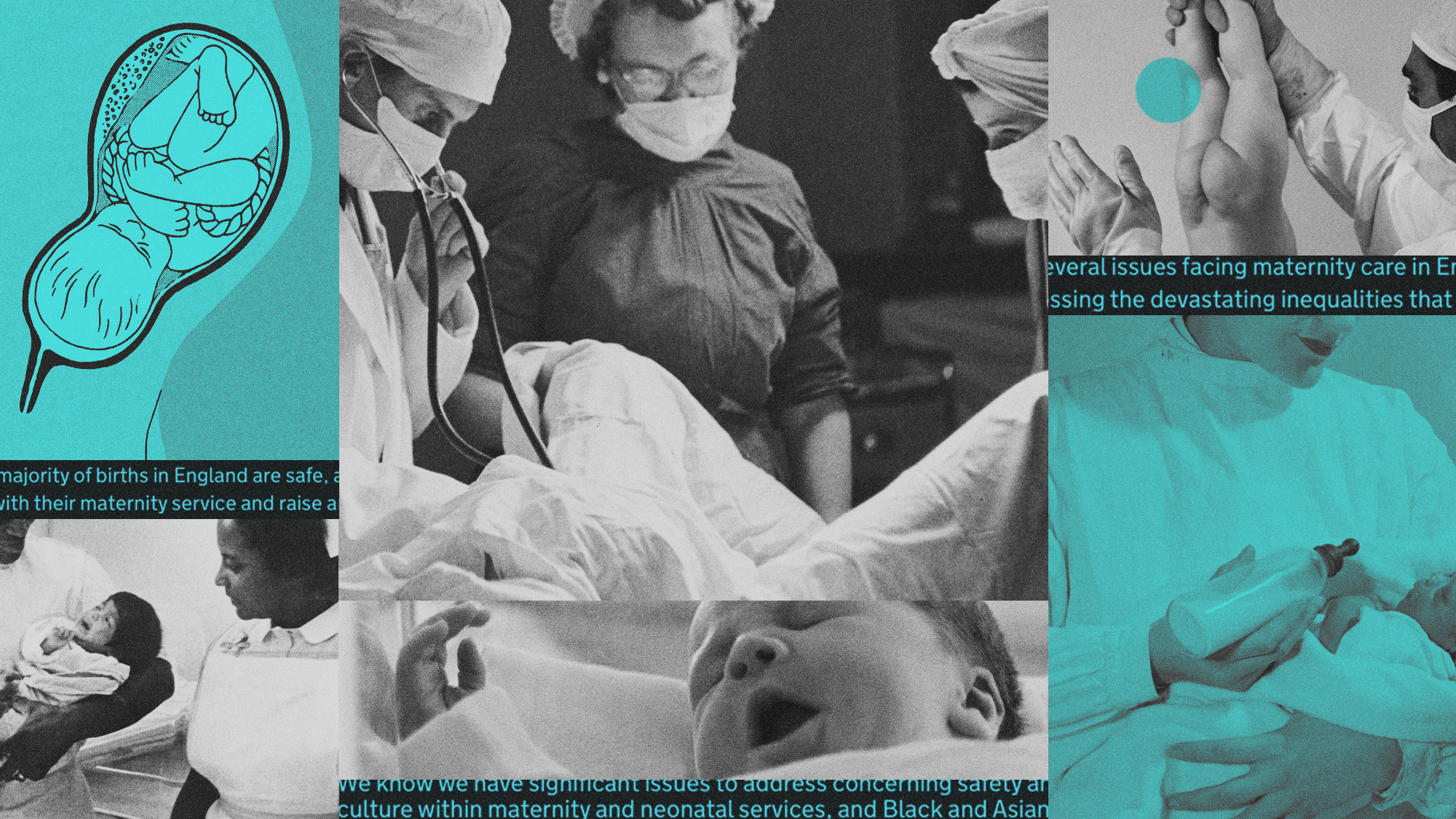
How did NHS maternity care get into such a state?
Interim report highlights discrimination and disregard for women’s choices, while experts warn of ‘culture of blame’
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
A series of high-profile scandals and independent reviews has painted a bleak picture of NHS maternity services. But Baroness Amos, who is leading the National Maternity and Neonatal Investigation into 12 NHS trusts, said “nothing” prepared her for the “unacceptable care families were receiving”. “I have been shocked,” she told Sky News, discussing her initial findings.
A “staggering” 748 recommendations have been made about maternity services in recent years, she said in an interim report. “Why are we in England still struggling to provide safe, reliable maternity and neonatal care everywhere in the country?”
What did the commentators say?
Amos found common themes: women being “disregarded” when they raised concerns, or not given the right information to make informed choices, as well as “discrimination against women of colour”, leading to far higher rates of maternal deaths, and similar prejudice against working-class and younger parents.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
The problem is “systemic”, said Hannah Barnes in The New Statesman. The Care Quality Commission found last year that nearly two-thirds (65%) of England’s maternity units required improvement or were inadequate. There is “something bigger going on – something unique that cannot simply be explained by staff shortages, low morale or a lack of funding”. Many hospitals with inadequate maternity units provide good care in other departments. “This is a problem of culture.”
One hospital under investigation for poor maternity care spent a decade pursuing a “normal birth” ideology, said The Sunday Times. Leeds Teaching Hospitals Trust’s maternity strategy directed services to “actively promote” vaginal births with “minimal medical interventions”. This has been “repeatedly blamed for contributing to poor care”, with staff waiting “too long to intervene”.
Between 2012 and 2023, the trust had “the lowest rates of caesarean sections in the country” – and its rate of stillbirths and newborn deaths “soared” to the highest. Other NHS trusts where inquiries into poor maternity care uncovered “catastrophic failures” have similar patterns.
The Royal College of Midwives abandoned its “normal birth” campaign in 2017. But a Sunday Times investigation last month found that almost two-thirds of universities still promote “normality” in midwifery courses. “It’s become like a religion,” said a senior midwife at a teaching hospital.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
Public inquiries have “repeatedly exposed systemic issues such as poor communication, a reluctance to learn from mistakes and knee-jerk defensiveness”, said lawyer Sara Stanger in The Times. The Ockenden review also noted that “midwives and obstetricians too often work in silos”, while concerns from families are “routinely downplayed or dismissed”.
But in my experience as health secretary, said Jeremy Hunt in The Guardian, “the biggest barrier to safer care in the NHS” was “a blame culture that stopped people being open about mistakes”. More than a third of NHS staff say they “don’t feel comfortable speaking up about safety concerns”. “That prevents professionals from learning from tragedies and condemns the system to repeating them.”
What next?
Amos’ investigation is due to publish its full report in the spring. But some victims say they are “disappointed” by the interim findings, said Sky News.
It appears to be “a bullet point list of failings that actually we’ve seen time and time again in independent reviews”, said Rebecca Matthews, who leads a campaign for families who claim they were failed by Oxford University Hospitals, one of the trusts Amos is investigating.
It seems as though it will lead to “some recommendations but no teeth”, she said. “We need some mechanisms that are going to hold people and systems to account.”
Previous reports have a “common message: policies and protocols alone cannot change outcomes”, said Stanger. Change “must start with trust and the freedom to speak up without fear of reprisal”.
Harriet Marsden is a senior staff writer and podcast panellist for The Week, covering world news and writing the weekly Global Digest newsletter. Before joining the site in 2023, she was a freelance journalist for seven years, working for The Guardian, The Times and The Independent among others, and regularly appearing on radio shows. In 2021, she was awarded the “journalist-at-large” fellowship by the Local Trust charity, and spent a year travelling independently to some of England’s most deprived areas to write about community activism. She has a master’s in international journalism from City University, and has also worked in Bolivia, Colombia and Spain.
-
 How the FCC’s ‘equal time’ rule works
How the FCC’s ‘equal time’ rule worksIn the Spotlight The law is at the heart of the Colbert-CBS conflict
-
 What is the endgame in the DHS shutdown?
What is the endgame in the DHS shutdown?Today’s Big Question Democrats want to rein in ICE’s immigration crackdown
-
 ‘Poor time management isn’t just an inconvenience’
‘Poor time management isn’t just an inconvenience’Instant Opinion Opinion, comment and editorials of the day
-
 ‘Zero trimester’ influencers believe a healthy pregnancy is a choice
‘Zero trimester’ influencers believe a healthy pregnancy is a choiceThe Explainer Is prepping during the preconception period the answer for hopeful couples?
-
 A Nipah virus outbreak in India has brought back Covid-era surveillance
A Nipah virus outbreak in India has brought back Covid-era surveillanceUnder the radar The disease can spread through animals and humans
-
 Is the US about to lose its measles elimination status?
Is the US about to lose its measles elimination status?Today's Big Question Cases are skyrocketing
-
 A real head scratcher: how scabies returned to the UK
A real head scratcher: how scabies returned to the UKThe Explainer The ‘Victorian-era’ condition is on the rise in the UK, and experts aren’t sure why
-
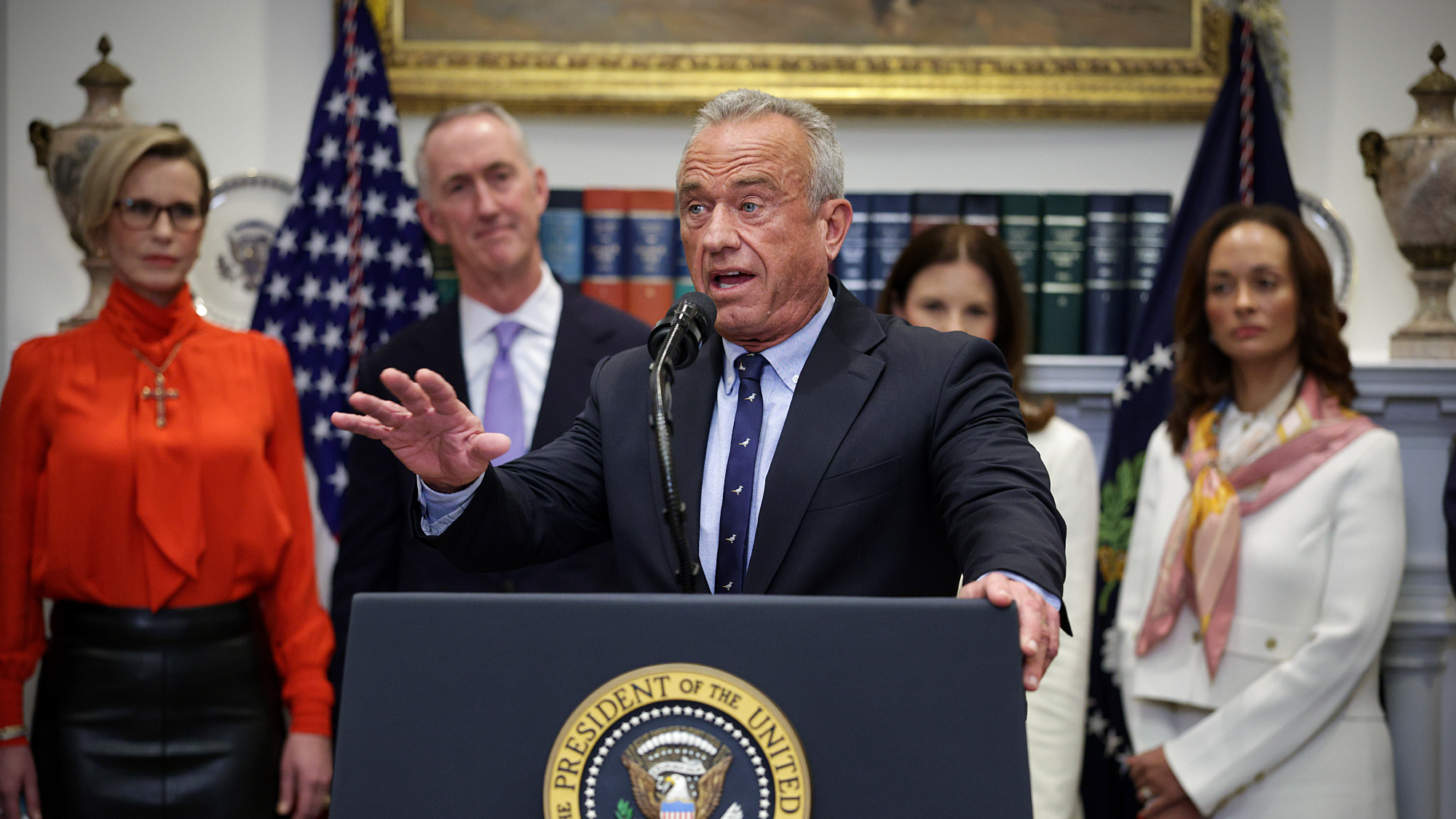
 Mixed nuts: RFK Jr.’s new nutrition guidelines receive uneven reviews
Mixed nuts: RFK Jr.’s new nutrition guidelines receive uneven reviewsTalking Points The guidelines emphasize red meat and full-fat dairy
-
 Trump HHS slashes advised child vaccinations
Trump HHS slashes advised child vaccinationsSpeed Read In a widely condemned move, the CDC will now recommend that children get vaccinated against 11 communicable diseases, not 17
-
 Deaths of children under 5 have gone up for the first time this century
Deaths of children under 5 have gone up for the first time this centuryUnder the radar Poor funding is the culprit
-
 How dangerous is the ‘K’ strain super-flu?
How dangerous is the ‘K’ strain super-flu?The Explainer Surge in cases of new variant H3N2 flu in UK and around the world