Private equity firms might be causing more deaths in hospital ERs
Deaths in ERs purchased by private equity firms rose 13%


A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
There has been a surge in recent years of private equity groups buying hospitals throughout the U.S., and emerging evidence suggests this may have unintended consequences. Following a hospital’s purchase by a private equity group, deaths in the emergency room increase significantly, according to new research. This data is adding to a slew of other health- and business-related complaints as more hospitals are being snapped up by private equity.
How much are deaths increasing at these hospitals?
After a private equity firm acquires a hospital, its emergency room death rate increases by 13.4%, or about seven additional deaths per 10,000 patients, according to research in the journal Annals of Internal Medicine. This data was based on “1,007,529 emergency department visits and 121,080 ICU hospitalizations across 49 private equity hospitals” from 2009 to 2019, said the journal. This was compared to data from 293 hospitals that were not acquired by private equity.
This is not the first study to find a link between private equity hospitals and ER deaths, but it “adds fresh evidence to previous studies showing harmful patient outcomes and higher costs among health care entities owned by profit-oriented financiers,” said NBC News. And this new research “differed from previous studies on private equity’s impact, which focused on patients who were admitted to the hospital” and not emergency rooms.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
The study also concluded that hospitals under the control of private equity firms have “reduced salaries and staffing relative to nonacquired hospitals,” said the journal. This could “explain the increased patient transfers to other hospitals, shortened ICU lengths of stay and increased emergency department mortality.”
Why is this happening?
The culprit is probably “decreases in overall staffing and salary expenditures,” said The Boston Globe. Private equity hospitals reduced ER salaries by 18.2% and ICU salaries by 15.9%, and this is “likely due to a combination of reducing staff and filling roles with less expensive — often meaning less experienced — labor.” This in turn has led to more deaths among these hospitals, and “deaths went up even as private equity acquired hospitals sent more of their sickest patients to other hospitals.”
This study “shows that those financial strategies may lead to potentially dangerous, even deadly consequences,” study author Dr. Zirui Song, a professor of health care policy at Harvard University and general internist at Massachusetts General Hospital, said to Newsweek. This is especially true among Medicare patients who are often “older and more vulnerable.”
This is at odds with the stated goal of private equity firms, experts say. “When private equity comes in, they try to jack up the revenues and then, when that reaches an endpoint, they start slashing expenses,” Dr. Robert McNamara, the chair of the department of emergency medicine at Temple University, said to NBC. Instead of “people just losing their jobs, you have bad patient outcomes here. Less staff equals worse outcomes.”
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
But even as this data is showing increased death rates, private equity hospitals aren’t going away. As of April 2025, approximately “488 U.S. hospitals are owned by private equity firms,” per the Private Equity Stakeholder Project. This includes 8.5% of all private hospitals and 22.6% of all for-profit hospitals; almost a quarter of these facilities, 22.6%, are also psychiatric hospitals. Many of these hospitals are also the only option for health care in their communities, as “27.7% of private equity-owned hospitals serve rural populations.”
Justin Klawans has worked as a staff writer at The Week since 2022. He began his career covering local news before joining Newsweek as a breaking news reporter, where he wrote about politics, national and global affairs, business, crime, sports, film, television and other news. Justin has also freelanced for outlets including Collider and United Press International.
-
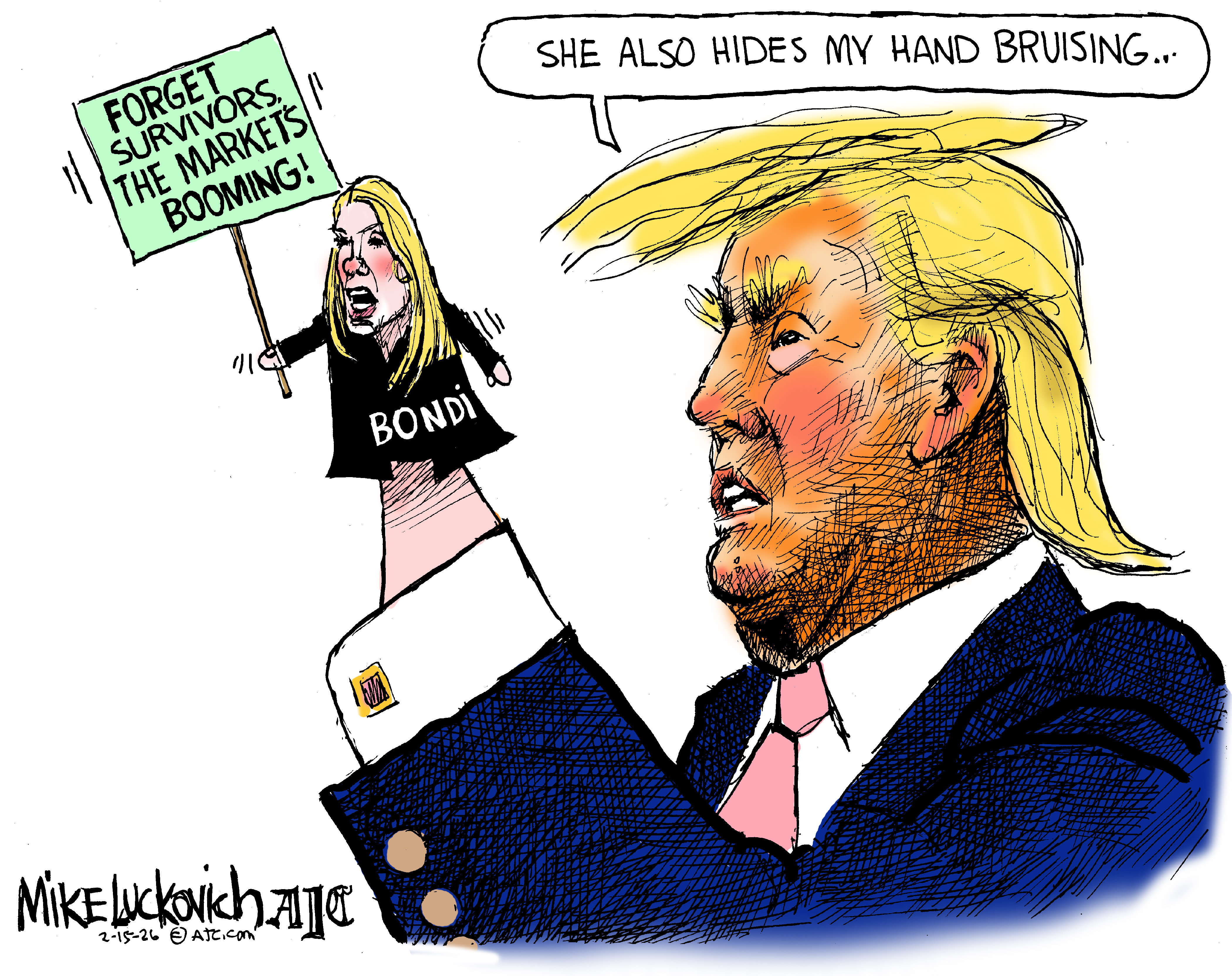 Political cartoons for February 15
Political cartoons for February 15Cartoons Sunday's political cartoons include political ventriloquism, Europe in the middle, and more
-
 The broken water companies failing England and Wales
The broken water companies failing England and WalesExplainer With rising bills, deteriorating river health and a lack of investment, regulators face an uphill battle to stabilise the industry
-
 A thrilling foodie city in northern Japan
A thrilling foodie city in northern JapanThe Week Recommends The food scene here is ‘unspoilt’ and ‘fun’
-
 ‘Zero trimester’ influencers believe a healthy pregnancy is a choice
‘Zero trimester’ influencers believe a healthy pregnancy is a choiceThe Explainer Is prepping during the preconception period the answer for hopeful couples?
-
 Growing a brain in the lab
Growing a brain in the labFeature It's a tiny version of a developing human cerebral cortex
-
 A Nipah virus outbreak in India has brought back Covid-era surveillance
A Nipah virus outbreak in India has brought back Covid-era surveillanceUnder the radar The disease can spread through animals and humans
-
 Is the US about to lose its measles elimination status?
Is the US about to lose its measles elimination status?Today's Big Question Cases are skyrocketing
-
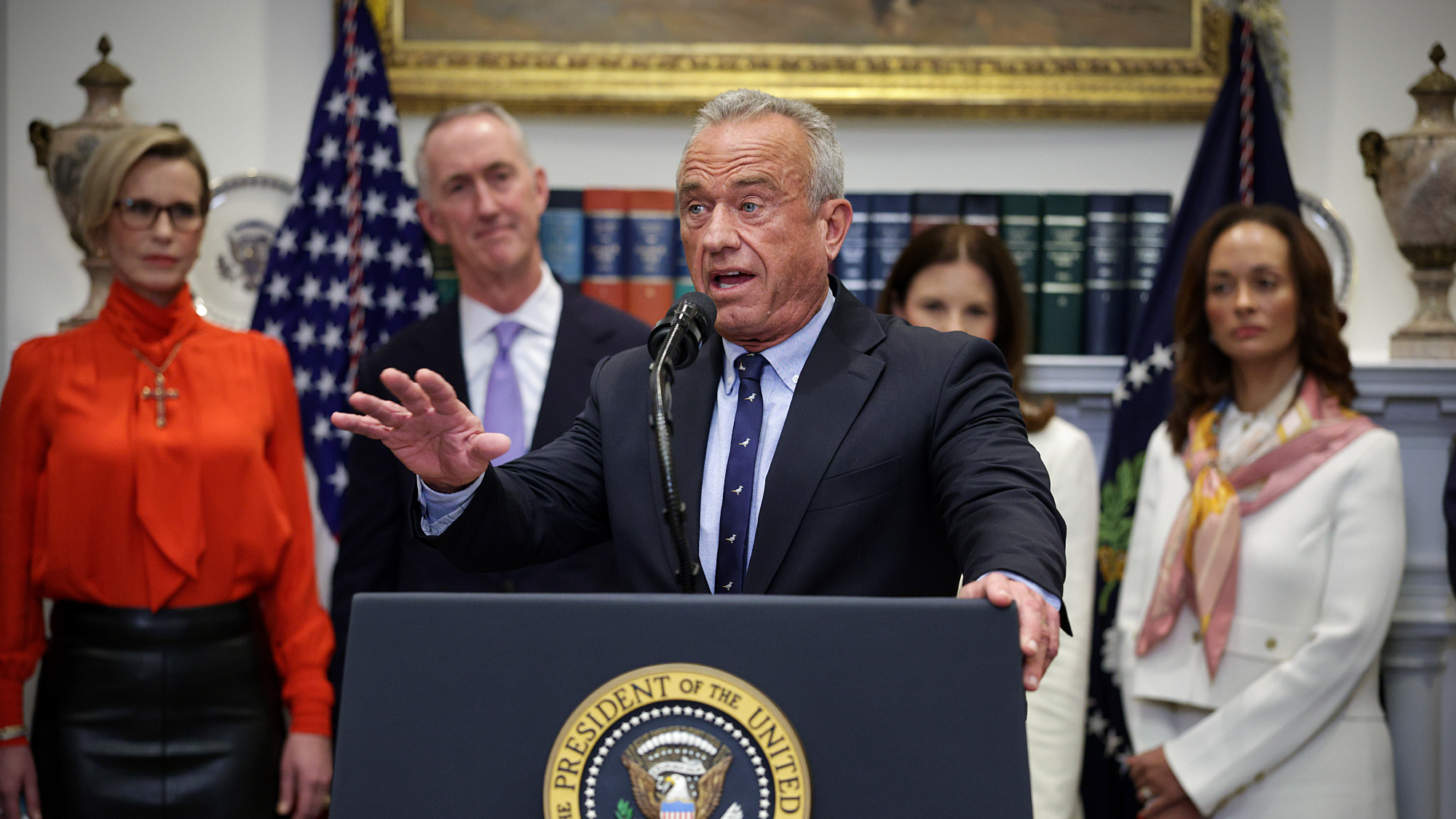
 Mixed nuts: RFK Jr.’s new nutrition guidelines receive uneven reviews
Mixed nuts: RFK Jr.’s new nutrition guidelines receive uneven reviewsTalking Points The guidelines emphasize red meat and full-fat dairy
-
 Trump HHS slashes advised child vaccinations
Trump HHS slashes advised child vaccinationsSpeed Read In a widely condemned move, the CDC will now recommend that children get vaccinated against 11 communicable diseases, not 17
-
 The truth about vitamin supplements
The truth about vitamin supplementsThe Explainer UK industry worth £559 million but scientific evidence of health benefits is ‘complicated’
-
 Deaths of children under 5 have gone up for the first time this century
Deaths of children under 5 have gone up for the first time this centuryUnder the radar Poor funding is the culprit
