The worsening state of the United States' maternal healthcare
The U.S. has the highest maternal mortality rate of any developed country. Why?


A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Since the pandemic, U.S. maternal mortality rates have soared and the problem is only getting worse. Here's everything you need to know:
Why does the U.S. have such a high maternal mortality rate?
According to the National Center for Health Statistics, the maternal mortality rate increased by 40 percent in 2021 compared to 2020, making the U.S. the country with the highest maternal mortality rate amongst developed countries. Maternal mortality, which refers to deaths due to complications from pregnancy or childbirth, also sees a wide discrepancy by race, with Black women recording a mortality rate double that of white women and Indigenous women at four times the rate, CNN reports.
"This is sort of my reflection on this time period, COVID-19 and pregnancy. Women were at increased risk for morbidity and mortality from COVID," Dr. Elizabeth Cherot, of the nonprofit March of Dimes told CNN. COVID exacerbated issues that were already present in the healthcare system. "In terms of issues of racial health inequities, of structural racism and bias, of access to health care, all of those factors that we know have played a role in terms of maternal mortality in the past continue to play a role in maternal mortality," said Dr. Chasity Jennings-Nuñez, chair of the perinatal/gynecology department at Adventist Health-Glendale.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
Additionally, maternal healthcare is worse in states with abortion bans following the overturning of Roe v. Wade (1973), per a report by the Gender Equity Policy Institute. The report found "people in banned and restrictive states have worse outcomes than their counterparts in supportive states," and that anti-abortion states "are less likely to enact policies, like paid parental leave, which have been shown to improve outcomes for new parents and babies."
How is U.S. maternal healthcare worsening?
More and more regions across the U.S. are finding themselves in maternal health "deserts." A 2022 study found that 36 percent of U.S. counties lack sufficient maternal health resources, impacting approximately 7 million women, NPR reports. A different study conducted in Louisiana tied maternal death and care access together concluding, "Risk of death during pregnancy and up to 1 year postpartum ... was significantly elevated among women residing in maternity care deserts compared with women in areas with greater access."
This is a problem that is only worsening. With the rise of anti-abortion laws, many maternal healthcare professionals are opting to move to locations without the laws. "Highly respected, talented physicians are leaving. Recruiting replacements will be extraordinarily difficult," said Bonner General Health, an Idaho hospital. The state has some of the most restrictive anti-abortion laws. "The Idaho Legislature continues to introduce and pass bills that criminalize physicians for medical care nationally recognized as the standard of care," the hospital continued in a news release. Leah Wilson, a doctor in Texas, explained that restrictive abortion laws "meant patients sitting there for days, actively losing nonviable pregnancies, and us waiting for something to go bad enough that we could help them."
The lack of proper healthcare coverage in these areas is complicating the problem. Experts are keeping an eye on five other states along with Idaho and Texas where maternal health could be deemed a crisis: Arkansas, Mississippi, Missouri, South Dakota, and Wisconsin. These states "have instituted abortion bans while keeping postpartum Medicaid coverage limited to 60 days," per Newsweek. By not extending healthcare coverage, many women would be forced to not seek necessary medical care. "Having any barrier to coverage in the postpartum setting is a direct barrier for accessing necessary care," explained Dr. Smita Carroll, an OB-GYN in New Mexico, to Newsweek.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
According to Carroll, "carrying a pregnancy to term has more risks than abortion care." Amy Chen, a senior attorney at the National Health Law Program (NHLP), added that "health care coverage is critical to catching and treating the health conditions and emergencies that are in part to blame for the United States' high maternal mortality and morbidity rates."
Unfortunately, a large number of those located in the care deserts are low-income and minority women located in rural areas. "In wealthier communities, private insurance helps offset low Medicaid payments to hospitals," writes The New York Times. "But in rural areas where poverty is more entrenched, there are too few privately insured patients."
What are possible solutions?
Maternal deaths are "largely preventable," according to Carroll, provided that Medicaid coverage is expanded to a year after birth. According to a report by the Center for American Progress as cited by Newsweek, "States hostile to abortion also have some of the highest rates of uninsured and comprise the majority of those still refusing to expand Medicaid."
"Physicians do not go to medical school and go into the practice of medicine because [they] enjoy interfacing with the legal profession," commented Katie McHugh, an OB-GYN from Indiana and board member of Physicians for Reproductive Health. Restrictive abortion laws end up tying the hands of physicians in terms of providing proper medical care. "Hospital closures, combined with the lack of access to outpatient and inpatient obstetrical care, results in the extremes of maternal and infant mortality that we see in my state," she added.
"What is just across the board hurting recruiting and retaining physicians right now is what's happening to reimbursement rates in Medicare and Medicaid," remarked Rep. Michael C. Burgess (R-Texas), who is also a trained OB-GYN, to Roll Call. "It is just phenomenally detrimental."
Devika Rao has worked as a staff writer at The Week since 2022, covering science, the environment, climate and business. She previously worked as a policy associate for a nonprofit organization advocating for environmental action from a business perspective.
-
 Local elections 2026: where are they and who is expected to win?
Local elections 2026: where are they and who is expected to win?The Explainer Labour is braced for heavy losses and U-turn on postponing some council elections hasn’t helped the party’s prospects
-
 6 of the world’s most accessible destinations
6 of the world’s most accessible destinationsThe Week Recommends Experience all of Berlin, Singapore and Sydney
-
 How the FCC’s ‘equal time’ rule works
How the FCC’s ‘equal time’ rule worksIn the Spotlight The law is at the heart of the Colbert-CBS conflict
-
 ‘Officials say exporters pay the tariffs, but consumers see the opposite’
‘Officials say exporters pay the tariffs, but consumers see the opposite’Instant Opinion Opinion, comment and editorials of the day
-
 Costco is at the center of an abortion debate
Costco is at the center of an abortion debateTalking Points The decision to no longer stock the abortion pill came following a pressure campaign by conservatives
-
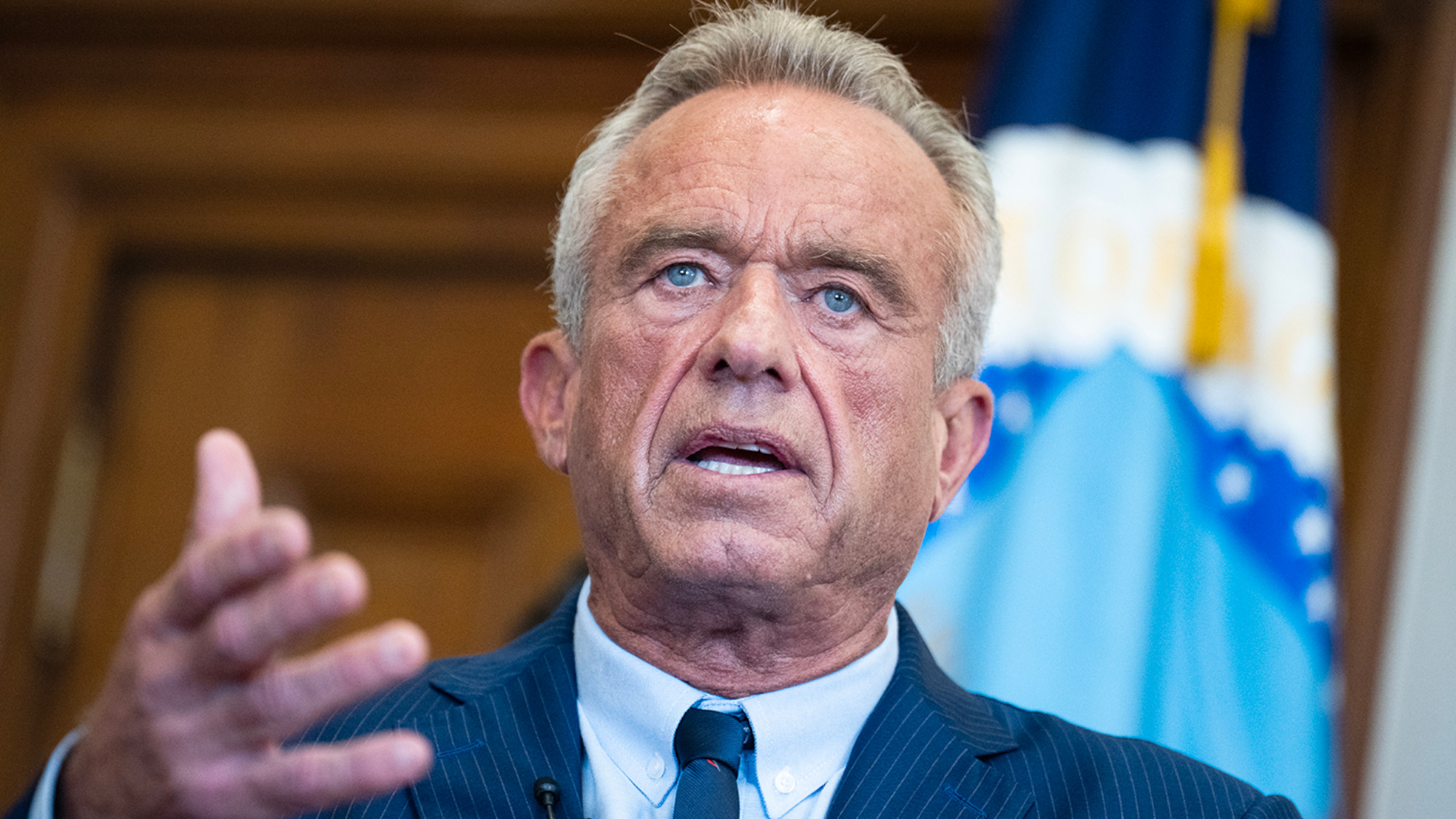 Health: Will medical science survive RFK Jr.?
Health: Will medical science survive RFK Jr.?Feature Robert F. Kennedy Jr. scrapped $500 million in mRNA vaccine research contracts
-
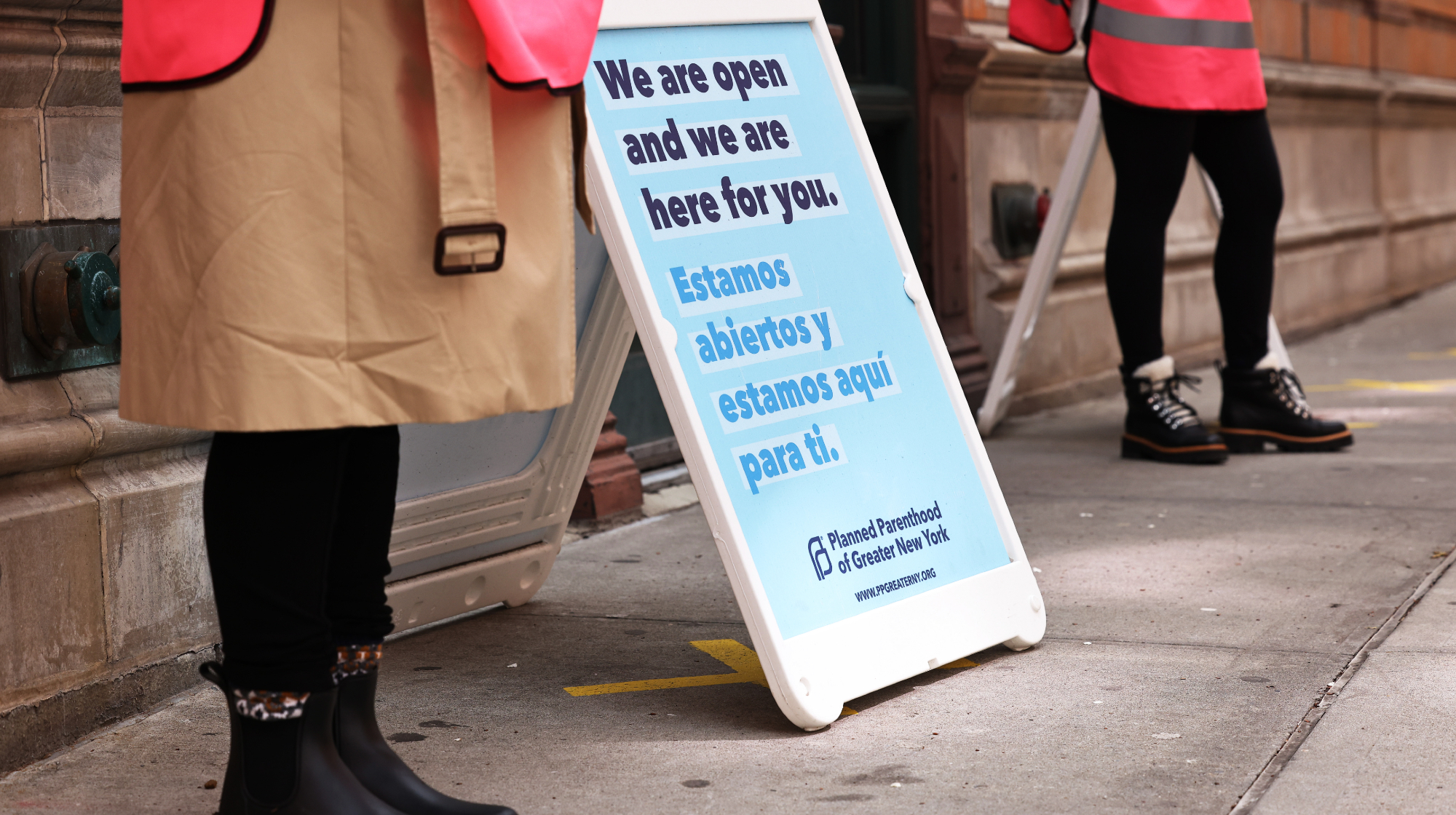 Judge halts GOP defunding of Planned Parenthood
Judge halts GOP defunding of Planned ParenthoodSpeed Read The Trump administration can't withhold Medicaid funds from Planned Parenthood, said the ruling
-
 'Singling out crypto for special scrutiny would be misguided'
'Singling out crypto for special scrutiny would be misguided'Instant Opinion Opinion, comment and editorials of the day
-
 The Supreme Court and Congress have Planned Parenthood in their crosshairs
The Supreme Court and Congress have Planned Parenthood in their crosshairsTalking Points Trump's budget bill and the court's ruling threaten abortion access
-
 Supreme Court lets states ax Planned Parenthood funds
Supreme Court lets states ax Planned Parenthood fundsSpeed Read The court ruled that Planned Parenthood cannot sue South Carolina over the state's effort to deny it funding
-
 The ambiguous legal state of ectopic pregnancy care
The ambiguous legal state of ectopic pregnancy careThe Explainer Rep. Kat Cammack's accusations of 'fearmongering' are the latest example of how mixed messages are complicating the debate around abortion
