NHS told to 'do God' to address needs of dying
New Nice guidelines say doctors should not be afraid to talk about personal beliefs

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Healthcare workers looking after dying patients in their final days must ask them about their spiritual beliefs, according to new NHS advice from the National Institute for Health and Care Excellence (Nice).
The guidance suggests "doctors must not be afraid to do God", reports the Daily Telegraph.
Officials say that in many cases patients don't want painkillers when they are dying, they want a priest, family member or even "their cat or dog by their bedside".
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
"Control of pain and other distressing symptoms is very important for dying people, but good end of life care goes far beyond that," said Sam Ahmedzai, emeritus professor of palliative medicine and a specialist member of Nice's quality standard committee.
"It includes asking about the dying person's spiritual, cultural, religious and social preferences."
The institute says that three quarters of the 500,000 annual deaths in England are anticipated.
Nice also reminded health and care workers that terminal patients should have their hydration needs assessed daily.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
"Under previous 'tick-box' rules, many thirsty patients were denied water and even treatment during their last days," says The Sun.
Professor Gillian Leng, deputy chief executive of Nice, said: "We know the vast majority of people in this country receive very good care at the end of life, but this isn't always the case.
"Our guidance will support doctors, nurses and other healthcare professionals so that they can work together to ensure that people die with dignity, whenever possible in the place of their choosing and with their symptoms effectively controlled."
The Church of England has welcomed the news. Reverend Dr Brendan McCarthy, its medical ethics adviser, said: "This guidance builds on Nice's 2011 recommendations for care at the end of life that highlighted the essential need for spiritual and religious care to be made available to all."
McCarthy said that it was "distressing" that "currently 85 per cent of patients in acute hospitals are not offered this care because their wishes are not sought."
The new Nice guidelines "underscore the vital role that chaplains play as part of a multi-disciplinary team in delivering holistic care at the end of life", he added.
-
 ‘Those rights don’t exist to protect criminals’
‘Those rights don’t exist to protect criminals’Instant Opinion Opinion, comment and editorials of the day
-
 Key Bangladesh election returns old guard to power
Key Bangladesh election returns old guard to powerSpeed Read The Bangladesh Nationalist Party claimed a decisive victory
-
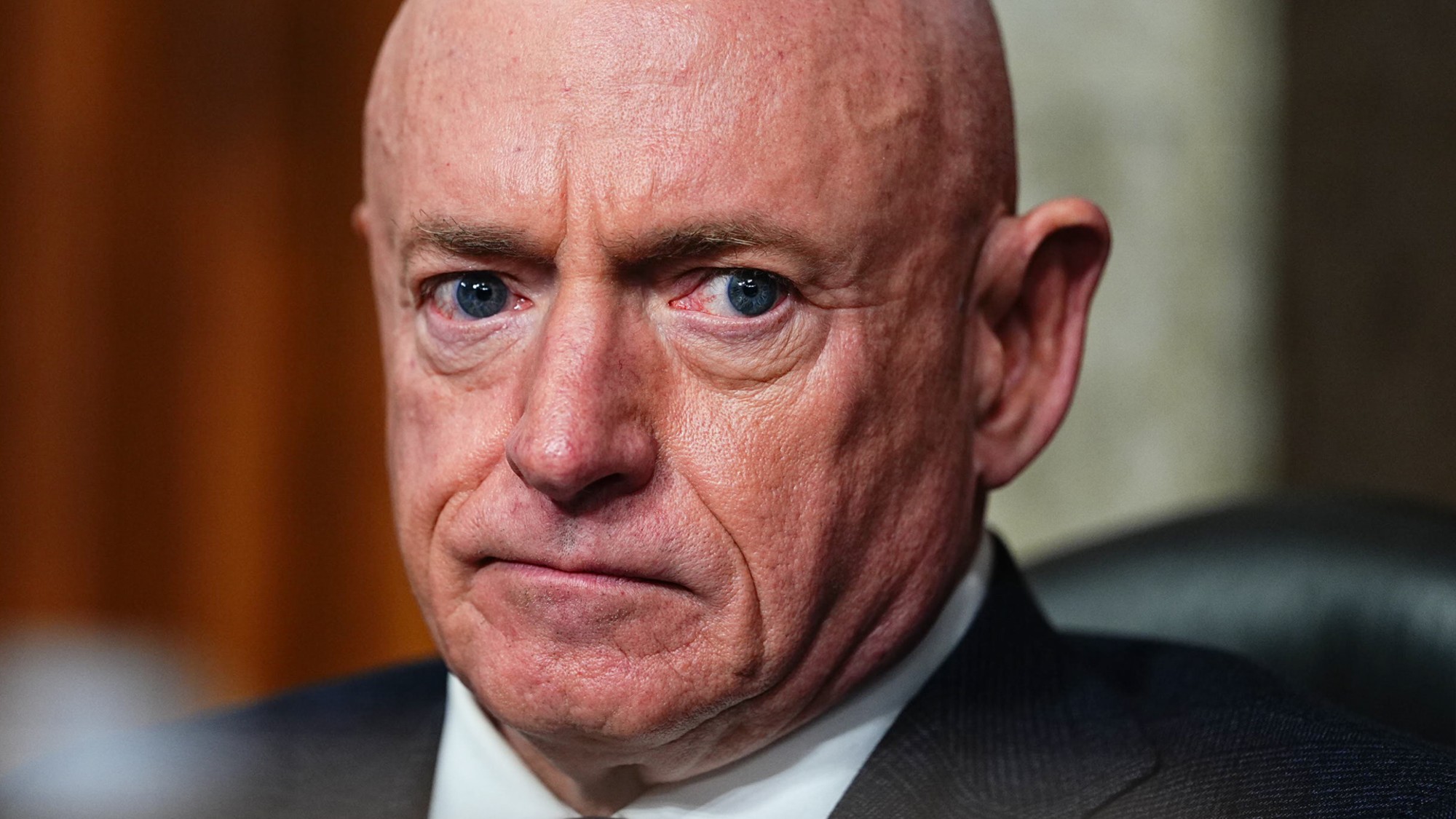 Judge blocks Hegseth from punishing Kelly over video
Judge blocks Hegseth from punishing Kelly over videoSpeed Read Defense Secretary Pete Hegseth pushed for the senator to be demoted over a video in which he reminds military officials they should refuse illegal orders
-
 A real head scratcher: how scabies returned to the UK
A real head scratcher: how scabies returned to the UKThe Explainer The ‘Victorian-era’ condition is on the rise in the UK, and experts aren’t sure why
-
 How dangerous is the ‘K’ strain super-flu?
How dangerous is the ‘K’ strain super-flu?The Explainer Surge in cases of new variant H3N2 flu in UK and around the world
-
 The ‘menopause gold rush’
The ‘menopause gold rush’Under the Radar Women vulnerable to misinformation and marketing of ‘unregulated’ products
-
 How the care industry came to rely on migrant workers
How the care industry came to rely on migrant workersThe Explainer Government crackdown on recruiting workers abroad risks deepening care sector crisis, industry leaders warn
-
 Could medics' misgivings spell the end of the assisted dying bill?
Could medics' misgivings spell the end of the assisted dying bill?Today's Big Question The Royal College of Psychiatrists has identified 'serious concerns' with the landmark bill – and MPs are taking notice
-
 Washwood Heath: Birmingham's pioneering neighbourhood health service
Washwood Heath: Birmingham's pioneering neighbourhood health serviceIn the Spotlight NHS England chair says there is a 'really good argument this is the model for the future'
-
 The UK's first legal drug consumption room
The UK's first legal drug consumption roomThe Explainer 'Potentially transformative moment in UK drugs policy' as The Thistle opens in Glasgow
-
 How can the UK solve the adult social care crisis?
How can the UK solve the adult social care crisis?Today's Big Question New commission announced to turn our buckling care sector around: yet more delay or finally a way forward?