Do unvaccinated COVID patients deserve scarce care? A doctor weighs in.
Justice, judgment, and the last ICU bed

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
COVID-19 has become, in the phrase of Centers for Disease Control Director Rochelle Walensky, "a pandemic of the unvaccinated." Six months after vaccines became widely available to the American public, nearly all those now hospitalized or dying from the illness never got their shot, some because they are too young or medically ineligible, and some by choice.
As hospitalizations surged in late summer and early fall, debate has roiled around whether it's ethical to deny care to the willfully unvaccinated in a triage situation. Should vaccine status be included in crisis standards of care, like those invoked in Alaska and Idaho? Should doctors make a moral judgment in apportioning scarce resources, instead of a purely medical one? Is that how we decide who gets the final intensive care unit (ICU) bed?
I explored this debate in an interview with Matthew Loftus, a writer and doctor who practices family medicine in Baltimore and Kenya. His tweets on the subject in late August caught my eye, particularly given what I knew of his writing on the ethics of vaccination and his clinical experience with addiction — a common analogy in the COVID triage debate — and communicable disease. Our conversation has been lightly edited for clarity and length.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
Let's start with the big question: Is it right to ration care according to vaccination status?
No. I don't think it's right to ration care according to vaccination status, at least as a general principle. There might be specific situations in which that could guide clinical decision making, but that's different.
I want to interrogate that with a couple arguments I've repeatedly seen around this issue. One is framed as a matter of justice. A good example appeared as an opinion piece in The Washington Post last week, where the author argued that usually it is "not the physician's place to judge" or provide care according to whether a patient's lifestyle choices contributed to their illness. But in times of crisis, she says, "we must ask: Is it fair to treat the person who chose to remain unvaccinated the same as someone who got the shot?" And her answer is: "Of course not," in fact, it "is ethically indefensible not to account for vaccination status" if you need a tiebreaker between two patients. I think that very simple appeal to fairness, to justice, resonates widely. And if you disagree, as it seems you do, how would you push back on that?
I would say there are a lot of other ways we ration care. I think every patient is different, and every patient is going to have a different set of risk factors. Especially when it comes to these really intense, life-saving interventions — CPR and intubation — we already try to avoid doing them for people whom we don't think they will help. We try not to intubate someone if we know we will never get that tube out while the patient is alive, for example. And so I think it makes more sense to admit, "Okay, yes, we always are trying to decide how to apportion care." It's always a judgment call whether or not and how we use these particular interventions.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You could imagine a scenario where you have two people who are otherwise exactly the same except for vaccination, where you could think about vaccination as a tiebreaker. But it's only in your imagination that you would have that scenario come up, and we already ration care in general in every health system everywhere, based on lots of different principles.
I also think it is unfair [to use vaccination status as the deciding factor], especially when you don't know why that person wasn't vaccinated. There are obviously people, like the picture in our mind — which I think is in many ways encouraged by different media portrayals and by people who enjoy fostering malice towards one another in our nation — the picture of someone who gets all their health information from their Aunt Gertrude on Facebook and is posting memes about [National Institute of Allergy and Infectious Diseases chief Anthony] Fauci being part of the Illuminati and whatnot.
But there are lots of different reasons people have chosen not to get vaccinated. I would say probably the biggest number I have encountered are people who got COVID and are hesitant about getting the vaccine because they're hesitant about reactions, or they know someone who had a bad reaction, or maybe they have a history of bad reactions. So for them, it's a matter of prudential judgment, but you can't look at that history when you're in the hypothetical ICU, you have one ventilator and two patients in front of you. Looking at someone's vaccination status, you can't say, "Oh, well, this person was vaccinated. They get the tube. This person was not vaccinated. They don't."
The person who was unvaccinated may have had legitimate concerns — and maybe concerns that I don't think overwhelm the moral case for getting vaccinated — but they did not necessarily embrace ignorance and maliciousness in deciding against vaccination.
So, this issue of justice and fairness: Would you say it's actually not just to ration care away from the unvaccinated? Or maybe it is just, but we have some other, higher duty, perhaps to mercy, or to human dignity, or something like that.
I think it is a matter of justice not to ration care away from the unvaccinated, because to do so, I think, is to pass a judgment on someone's other personal health decisions that we would never apply in any other case. All health care is a mixture of trying to provide justice while also being merciful to others. It's impossible to be a good health-care worker and not be willing to be merciful with people who, quite frankly, got themselves into the trouble that they're in and had many opportunities not to do so. But it's also a matter of justice in giving that person what they need to survive or, if not to survive, to die in a way that honors the person they are.
So maybe the issue of justice is about care for the unvaccinated person and not (or not exclusively) about being fair to the vaccinated person by elevating COVID vaccination to a be-all and end-all qualifying factor in a way we wouldn't with other medical concerns — of which there are many — that patient behavior affects.
Yeah. I think that's a good way of putting it. And I think people are concerned because COVID is a unique stressor. People who choose to be unvaccinated without any genuine, compelling reason are putting additional strain on the health-care system in ICUs everywhere. And I think that that's just a unique thing that we're dealing with right now. But again, people who do all sorts of terrible things are constantly straining emergency rooms and putting other burdens and driving all of our health-care premiums up, and we're not having a conversation about it.
We just don't see it, so we're not talking about it in public the same way.
Yeah, exactly.
This is a good place to bring up the other counterargument I wanted to mention, which is this analogy to drug addiction or other addictions. (Your discussion of that on Twitter was what first gave me the idea for this interview.) And for someone with a lay-level understanding of addiction, I think the analogy makes a lot of sense. I've read comments like, "Well, you wouldn't give a lung transplant to someone who won't stop smoking," or, "You wouldn't give a heart transplant to someone who's using cocaine every day, so you shouldn't give that ICU bed to the willfully unvaccinated." Do you think the addiction analogy has value? Or are these situations not actually similar?
I think that the analogy has partial value. All health conditions are different. All behavioral inputs into our health conditions are different, and so of course the analogy will break down at some point. And again, I think there tends to be this fixation on the people who are ignorant and proud of it — especially with that Herman Cain Award site, it's just ghoulish. [Loftus is referring to the Herman Cain Award subreddit, which mocks those who die of or lose loved ones to COVID-19 after publicly deriding vaccination, usually on social media.]
So, in general, the principal still stands that we ought to give people the health care they need to survive, to flourish, and once we've figured out what that is, then we work backwards from that to say, "Okay, so which of these interventions can do that in the most cost-effective method?" And that's how every place, every country in the world, all the time, that has some rhyme and reason to their health care decides how to apportion their health care: what to pay for, what to give people.
Lastly, you've mentioned several times the idea that there's a degree, perhaps, of resentment or schadenfreude, or even simple anger dressed up — maybe consciously, maybe not — in these nobler sentiments about being fair. How much of this debate would you say is those other things going on under the surface (or maybe not-so-under-the surface, as with the Herman Cain Award subreddit), and how much is just a sincere, well-intended difference in ethical judgment calls?
It's a good question, and one I wish I could cover with an answer, but I don't think I can say for sure.
I think for many, wanting to reserve care for the vaccinated is probably directly correlated to how much they have suffered because of the pandemic. I think about health-care workers who were just starting to breathe a sigh of relief and are now experiencing all of the same terrible things that they experienced at the height of the pandemic before vaccines were available. For them, it is probably more of that what I would call a righteous anger, and a sense of justice, of longing to care for their patients who don't have COVID, or who have COVID and are vaccinated, and wanting them to get the best care they can — but instead having all their energy being taken up by these unvaccinated and hospitalized patients.
And I suspect there's also the people who are most online and who are already polarized, shall we say, and these are the people who are probably most stuck in unrighteous anger, and just — well, being a part of a mob feels fun. That's why people keep doing it. And I think that's what's happening with some people who don't have so much of a personal connection to the pandemic and are just enjoying watching people suffer for their bad decisions.
Bonnie Kristian was a deputy editor and acting editor-in-chief of TheWeek.com. She is a columnist at Christianity Today and author of Untrustworthy: The Knowledge Crisis Breaking Our Brains, Polluting Our Politics, and Corrupting Christian Community (forthcoming 2022) and A Flexible Faith: Rethinking What It Means to Follow Jesus Today (2018). Her writing has also appeared at Time Magazine, CNN, USA Today, Newsweek, the Los Angeles Times, and The American Conservative, among other outlets.
-
 What is the endgame in the DHS shutdown?
What is the endgame in the DHS shutdown?Today’s Big Question Democrats want to rein in ICE’s immigration crackdown
-
 ‘Poor time management isn’t just an inconvenience’
‘Poor time management isn’t just an inconvenience’Instant Opinion Opinion, comment and editorials of the day
-
 Bad Bunny’s Super Bowl: A win for unity
Bad Bunny’s Super Bowl: A win for unityFeature The global superstar's halftime show was a celebration for everyone to enjoy
-
 A Nipah virus outbreak in India has brought back Covid-era surveillance
A Nipah virus outbreak in India has brought back Covid-era surveillanceUnder the radar The disease can spread through animals and humans
-
 Covid-19 mRNA vaccines could help fight cancer
Covid-19 mRNA vaccines could help fight cancerUnder the radar They boost the immune system
-
 The new Stratus Covid strain – and why it’s on the rise
The new Stratus Covid strain – and why it’s on the riseThe Explainer ‘No evidence’ new variant is more dangerous or that vaccines won’t work against it, say UK health experts
-
 RFK Jr. vaccine panel advises restricting MMRV shot
RFK Jr. vaccine panel advises restricting MMRV shotSpeed Read The committee voted to restrict access to a childhood vaccine against chickenpox
-
 RFK Jr. scraps Covid shots for pregnant women, kids
RFK Jr. scraps Covid shots for pregnant women, kidsSpeed Read The Health Secretary announced a policy change without informing CDC officials
-
 New FDA chiefs limit Covid-19 shots to elderly, sick
New FDA chiefs limit Covid-19 shots to elderly, sickspeed read The FDA set stricter approval standards for booster shots
-
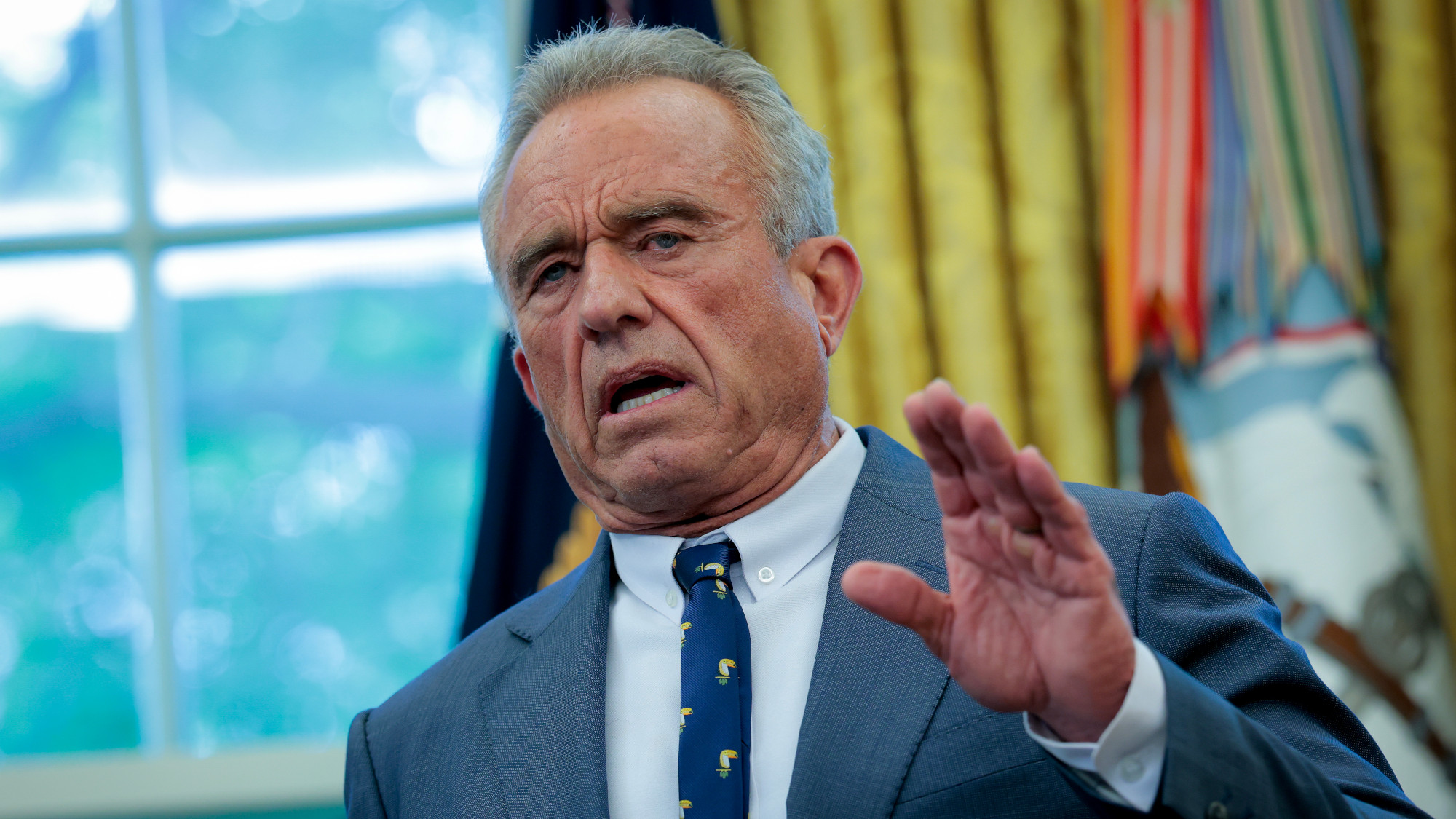 RFK Jr.: A new plan for sabotaging vaccines
RFK Jr.: A new plan for sabotaging vaccinesFeature The Health Secretary announced changes to vaccine testing and asks Americans to 'do your own research'
-
 Five years on: How Covid changed everything
Five years on: How Covid changed everythingFeature We seem to have collectively forgotten Covid’s horrors, but they have completely reshaped politics
