The dark side of the contraceptive coil
Study linking hormonal IUD to increased breast cancer risk adds to growing concerns about the coil
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Hormonal coils have become increasingly popular in recent years, but a recent study found an unexpected association between the hormonal coil and an increased risk of breast cancer.
Although the cancer risk unearthed by the study, published last week in the journal Jama, was low overall, and extremely low for women under 30, the negative headlines are the latest example of a slew of bad PR around the contraceptive coil.
'Highly unexpected'
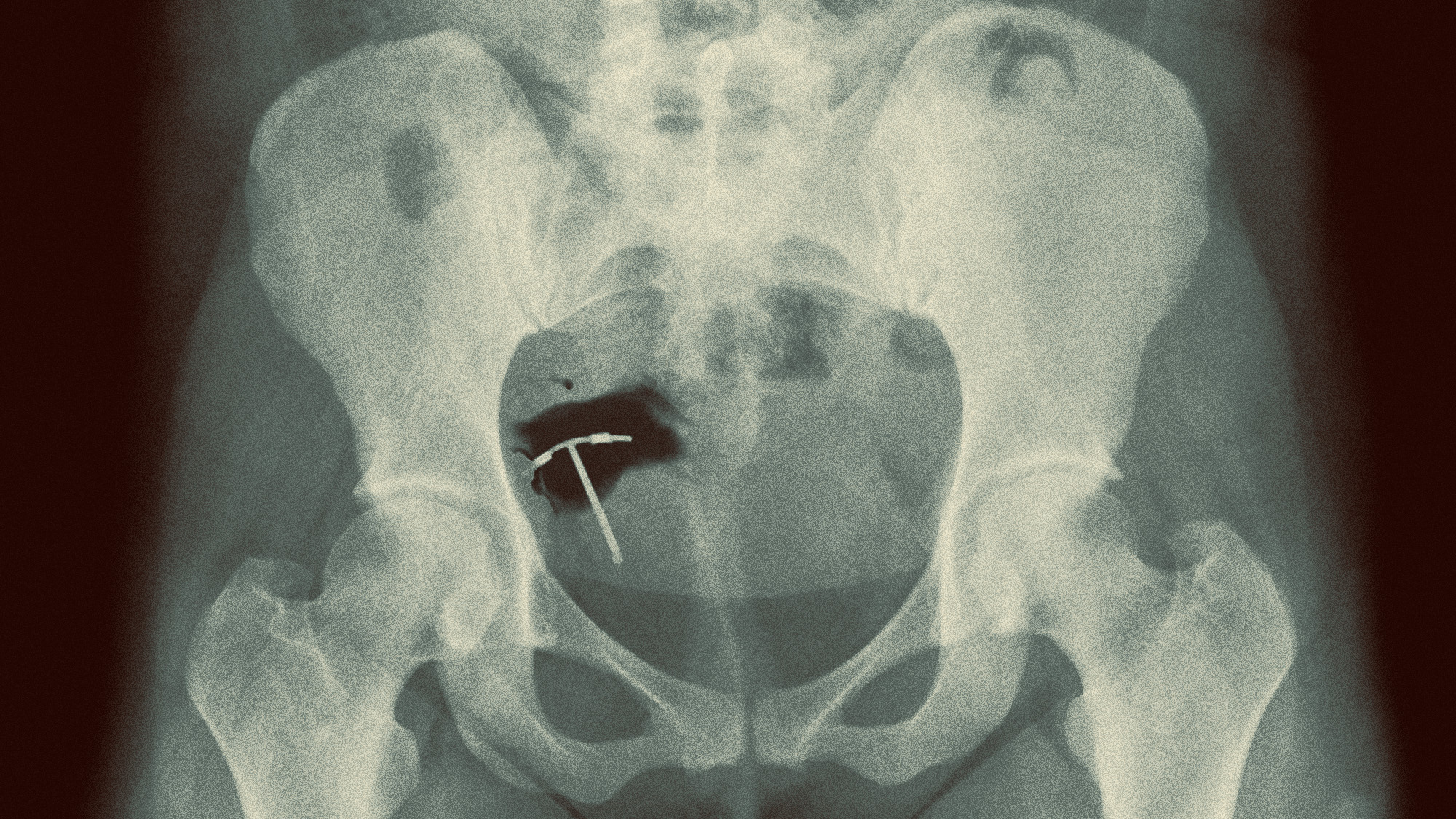
Hormonal coils, which release low levels of hormones into the body, are one of two types of contraceptive intrauterine device (IUD). The other is the so-called "copper" coil, which doesn't release hormones into the body.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
Researchers compared nearly 80,000 women in Denmark between the age of 15 and 49 who had used hormonal coil for five years, with the same number of similar women without the coil. Those with the coil had a 40% higher chance of developing breast cancer, said The New York Times.
The oral contraceptive pill has long been known to have a similar risk factor – but the assumption had always been that the coil would not increase the risk, because of the lower levels of hormones released. The results are "highly unexpected", Dr Channa Jayasena, from Imperial College London, told The Independent.
And they need to be taken "seriously", especially among women over 30, when the risk of breast cancer increases, said Lina Morch, from the Danish Cancer Institute, who led the study.
'Consistently underestimated' pain
More than three-quarters of women find getting a coil fitted moderately or severely painful, a study in the Journal of Family Planning and Reproductive Health Care found. Research has long shown that doctors severely underestimate the pain of insertion.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
"Sometimes I joke that if men were having this procedure, it would be done under general anaesthesia," Jessica Horwitz, from the US women's health care clinic Tia, told Cosmopolitan. But "many (if not most) doctors still tell patients that IUD insertion involves just 'some discomfort'".
The NHS advises that extra pain relief should be available on request. But this is "not always the case", said Elle, and many clinics and GP practices do not offer local anaesthetic. "'Come with me to get an IUD' has become a popular format" on TikTok – and it's "hardly surprising", given that women's pain has "consistently been underestimated".
Desperate times, DIY measures
More than a million women in the UK have a coil, and about 45,000 are fitted every year. Waiting lists for gynaecological procedures have increased by 60% since pre-pandemic levels, with the average waiting time for fitting or removing the coil on the NHS now ranging from four weeks to more than 12, said Mail Online.
The situation is exacerbated by the fact that some GP surgeries have stopped fitting or removing coils as training doctors to do so is "both lengthy and expensive", and many sexual health clinics have closed due to funding cuts.
Now, experts are pointing to the growing number of women who, without any alternative, "feel forced to remove their own coils", with the "DIY IUD removal" trend taking off on TikTok over the past few years. Doctors warn that removing the coil yourself can damage the cervix or uterus, and risks severe pain, heavy bleeding and infection – even cervical shock and pelvic disease.
"We know that many women are having to wait too long to have a coil fitted or removed, which is simply unacceptable," said Geeta Kumar, vice-president of the Royal College of Obstetricians and Gynaecologists . "The new government must address this issue by investing in time for GPs to undergo training on fitting coils."
Harriet Marsden is a senior staff writer and podcast panellist for The Week, covering world news and writing the weekly Global Digest newsletter. Before joining the site in 2023, she was a freelance journalist for seven years, working for The Guardian, The Times and The Independent among others, and regularly appearing on radio shows. In 2021, she was awarded the “journalist-at-large” fellowship by the Local Trust charity, and spent a year travelling independently to some of England’s most deprived areas to write about community activism. She has a master’s in international journalism from City University, and has also worked in Bolivia, Colombia and Spain.