The pros and cons of getting a vasectomy
Male sterilisation is considered highly safe and reliable, but not always reversible, painless or accessible
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
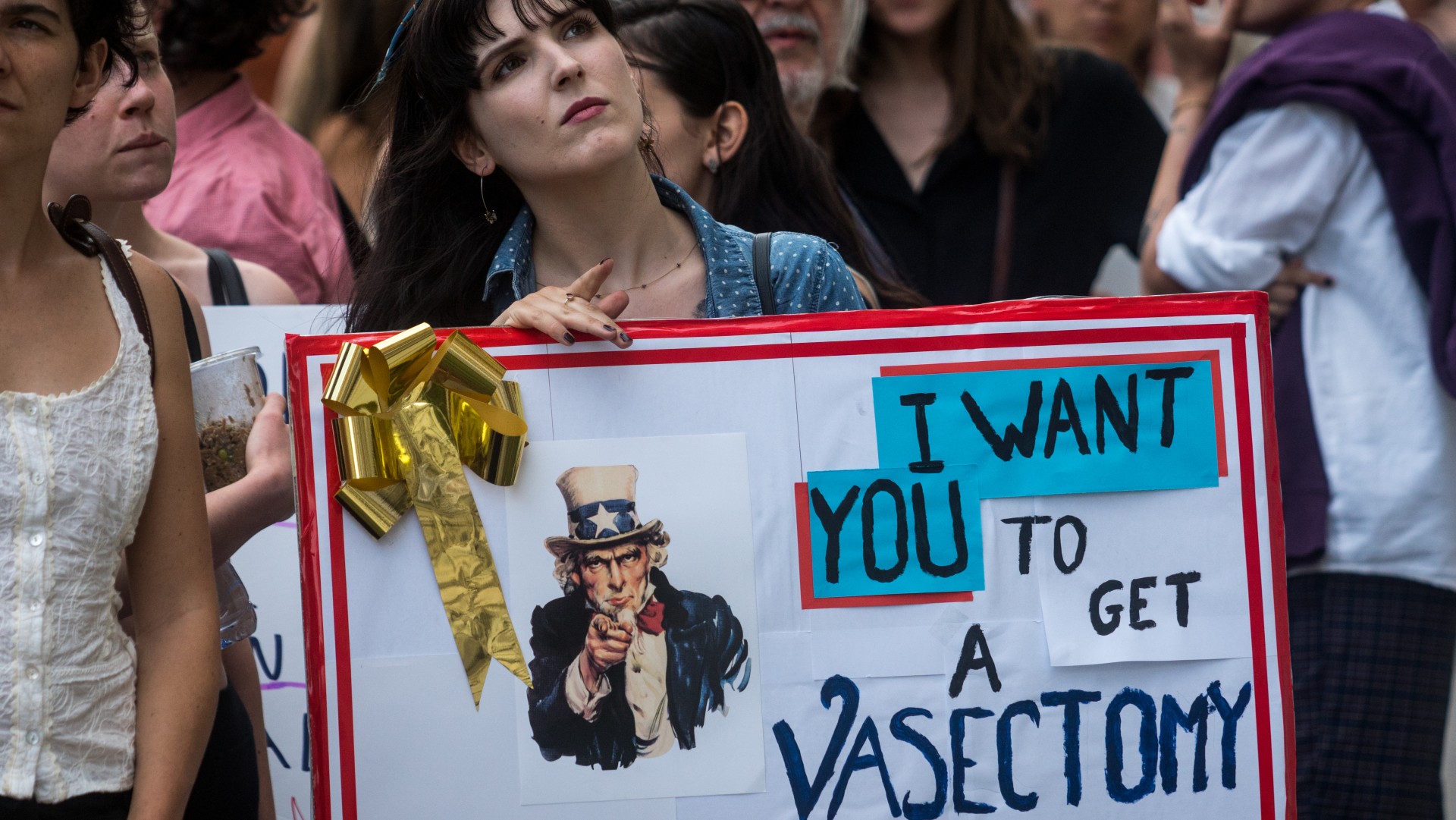
Interest in vasectomies, or male sterilisation, as a contraceptive method is growing worldwide, particularly in the US where the overturning of Roe v. Wade has dramatically restricted abortion access.
Within a week of the Supreme Court decision in 2022, daily online searches for “vasectomy” nearly doubled, according to a report by telehealth company Innerbody Research. Searches for “where can I get a vasectomy” increased by 850% in some states, the report said. Some men in the US are now uploading footage of their vasectomies to TikTok.
In the decade prior to 2015 there had been a long-term decline in the number of vasectomies performed in the UK, falling 64% according to NHS Digital data. But last year there were “anecdotal reports” that vasectomies for young men were becoming more prevalent in the UK and even in China, said BBC Worklife, “where sterilisation remains culturally taboo”. In Australia, where vasectomy rates are relatively high compared with other developed nations, a doctor told SBS News that there had been “close to 20% increase in the number of childless men under 30 requesting vasectomies” between 2020 and 2021.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
“It’s a big decision to have a vasectomy,” said the NHS. The Week takes a look at some of the main pros and cons of the procedure.
1. Pro: safer than reported
A vasectomy is a surgical procedure to cut or block the tubes that carry a man’s sperm from the testicles to the penis, in order to “permanently prevent pregnancy”, according to the NHS.
Vasectomies are “much safer than reported”, said a team of UK doctors who checked 94,000 procedures for complications. At the European Association of Eurology medical conference last month, the team said “serious risks are extremely rare”, according to BBC News.
Only about two in every 1,000 (0.2%) men experienced extreme scrotal pain, which contradicts a “commonly used” patient information leaflet that puts the figure at up to one in 20, it said. Rates of infection were just over 1%.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
“Vasectomy is a very reliable and safe contraception method,” said senior NHS registrar Julian Peacock, who headed the review. He pointed out that the risk information on patient leaflets is from the 1980s, and is now outdated.
Vasectomies do not cause any increased risk of developing prostate cancer, according to two US studies published in the Journal of Clinical Oncology in 2016.
Vasectomies do not affect sexual performance, sex drive, increase risk of heart disease or cause severe pain, said the Mayo Clinic.
2. Con: some risks and pain
“Your ball sack (scrotum) may become bruised, swollen or painful,” according to the NHS. “Some men have ongoing pain in their testicles.”
There is “a low risk of complications or side effects”, said the Mayo Clinic, but possible side effects can include bleeding or a scrotal blood clot, blood in the semen, infection and in rare cases, fluid build-up or an abnormal cyst in the testicle.
However, there are two types of vasectomy: a conventional procedure using a scalpel (surgical knife) and a so-called no-scalpel, or “blood-free” or snipless vasectomy. A no-scalpel vasectomy is associated with far fewer risks and pain.
Last week, a no-scalpel vasectomy passed a preliminary clinical test in the US, reported MedPage Today, achieving a decrease in sperm of almost 100% after 30 days, and causing no serious side effects.
3. Pro: quick and simple
“Once perceived as drastic and irreversible, vasectomy surgeries are now simple, routine and relatively painless,” according to The Guardian. “Urologists advertise ‘no needle, no scalpel’ procedures.”
The procedure involves “a small cut or puncture in the skin of the scrotum, which can be closed with dissolving stitches”, BBC News said. A day or two of rest is recommended, and sport, heavy lifting and sex should be avoided for at least a week.
“It’s usually carried out under local anaesthetic, where you’re awake but don’t feel any pain, and takes about 15 minutes,” NHS guidance said.
4. Con: not always reversible
According to the American Urological Assocation, between 3 and 6% of the 300,000 vasectomy patients each year in the US want to reverse the procedure.
Vasectomies “should be thought of as a permanent procedure for those considering it”, said Science Focus.
The success rates of a reversal are “not high”, according to Science Focus – about 75% “if done within three years of the original procedure, falling to around 55% up to eight years, and 40% up to 14 years”.
“A reversal to restore fertility will not always work,” said BBC News, “and is likely to have to be carried out privately, which could cost thousands of pounds.”
Reversal works by rejoining the tubes that carry sperm from the testes to the penis. There are two techniques: macroscopic vasovasostomy, performed with the naked eye; and microscopic vasovasostomy, using strong magnification.
A review published in the SN Comprehensive Clinical Medicine in 2021 showed a higher success rate of reversal with the microscopic procedure: 91.4% patency (being open or unobstructed) after the operation, compared with 80.5% for the macroscopic procedure.
A non-surgical vasectomy, called RISUG (reversible inhibition of sperm under guidance) is also under development in India. It involves injecting a gel into the vas deferens to block sperm, rather than cutting or tying it. A shot can then break down the gel. Vasagel, the US equivalent, is currently in clinical trials, reported Healthline.
5. Pro: reliable and effective
“The most reliable means of contraception for men – and one that cannot fail or be forgone in the heat of the moment – is a vasectomy,” said The Economist.
Vasectomy has a 0.15% failure rate at preventing pregnancy, according to the Centers for Disease Control and Prevention, making it highly effective compared with other forms of contraception.
“It usually succeeds,” said Michelle Roberts, digital health editor for the BBC, “but doctors advise using contraception for a few months as some sperm can still be present.”
6. Con: not always accessible or affordable
“In most parts of the UK, a vasectomy is available free of charge from the NHS,” said official guidance. “But waiting lists can be several months, depending on where you live.”
Doctors could also refuse to refer you for the procedure.
“If you’re under 30, you’ll find many surgeons are reluctant to do it”, the NHS said. “You may be more likely to be accepted for a vasectomy if you’re over 30 and have had children.”
Cost in England “may be becoming an issue”, said The Guardian in 2016. “At a time of increasing financial pressure on the NHS, some clinical commissioning groups are considering reducing the number of vasectomies they will pay for, or dropping them altogether.”
In the US, a vasectomy can cost up to $1,000, according to Planned Parenthood, although they can be free depending on health insurance or government programs like Medicaid. But a vasectomy “usually ends up saving you money in the long run,” the guidance adds.
Harriet Marsden is a senior staff writer and podcast panellist for The Week, covering world news and writing the weekly Global Digest newsletter. Before joining the site in 2023, she was a freelance journalist for seven years, working for The Guardian, The Times and The Independent among others, and regularly appearing on radio shows. In 2021, she was awarded the “journalist-at-large” fellowship by the Local Trust charity, and spent a year travelling independently to some of England’s most deprived areas to write about community activism. She has a master’s in international journalism from City University, and has also worked in Bolivia, Colombia and Spain.
-
 How the FCC’s ‘equal time’ rule works
How the FCC’s ‘equal time’ rule worksIn the Spotlight The law is at the heart of the Colbert-CBS conflict
-
 What is the endgame in the DHS shutdown?
What is the endgame in the DHS shutdown?Today’s Big Question Democrats want to rein in ICE’s immigration crackdown
-
 ‘Poor time management isn’t just an inconvenience’
‘Poor time management isn’t just an inconvenience’Instant Opinion Opinion, comment and editorials of the day
-
 ‘Zero trimester’ influencers believe a healthy pregnancy is a choice
‘Zero trimester’ influencers believe a healthy pregnancy is a choiceThe Explainer Is prepping during the preconception period the answer for hopeful couples?
-
 Stopping GLP-1s raises complicated questions for pregnancy
Stopping GLP-1s raises complicated questions for pregnancyThe Explainer Stopping the medication could be risky during pregnancy, but there is more to the story to be uncovered
-
 Choline: the ‘under-appreciated’ nutrient
Choline: the ‘under-appreciated’ nutrientThe Explainer Studies link choline levels to accelerated ageing, anxiety, memory function and more
-
 The controversial Free Birth Society
The controversial Free Birth SocietyThe Explainer Influencers are encouraging pregnant women to give birth without midwife care – at potentially tragic cost
-
 The rise in unregulated pregnancy scans
The rise in unregulated pregnancy scansUnder The Radar Industry body says some private scan clinics offer dangerously misleading advice
-
 Cytomegalovirus can cause permanent birth defects
Cytomegalovirus can cause permanent birth defectsThe Explainer The virus can show no symptoms in adults
-
 RFK Jr. scraps Covid shots for pregnant women, kids
RFK Jr. scraps Covid shots for pregnant women, kidsSpeed Read The Health Secretary announced a policy change without informing CDC officials
-
 The UK's first baby born to woman with womb transplant
The UK's first baby born to woman with womb transplantThe Explainer 'Astonishing' medical breakthrough, the culmination of 25 years of research, could pave the way for more procedures to combat uterine infertility