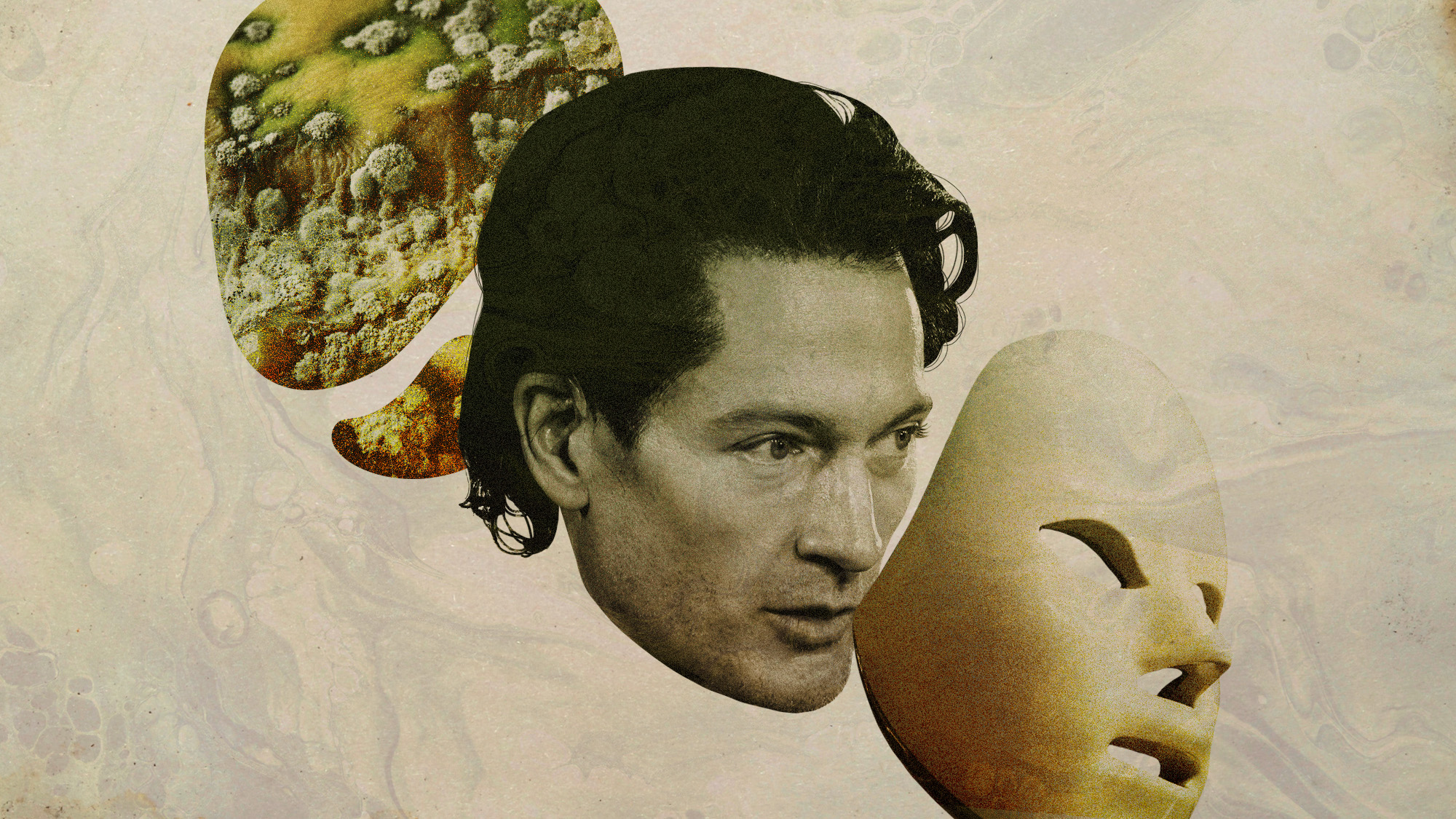
Coronavirus: the psychological illnesses that can be triggered by Covid
New study finds that one in five patients infected with the virus go on to suffer from mental disorder

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Almost 20% of coronavirus patients are diagnosed with a psychiatric disorder or mental health issue within three months of testing positive for Covid-19, a new study has found.
The research, outlined in a paper in The Lancet, adds to the growing list of “long Covid” symptoms being reported. Experts have warned that “action is needed to mitigate the mental health toll” of the global pandemic, says The Guardian.
Increased risk
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
Researchers from the University of Oxford and NIHR Oxford Health Biomedical Research Centre analysed the health records of almost 70 million people in the US and found that nearly one in five who had tested positive for the new coronavirus were then diagnosed with a mental illness within 14 to 90 days.
The analysis included data on “more than 62,000 cases of Covid-19 that did not require a hospital stay or an emergency department visit”, The Guardian reports.
The study also found that the correlation between mental illness and coronavirus goes both ways: people with professionally diagnosed pre-existing mental health disorders were about 65% more likely to be diagnosed with Covid-19 than people without.
It is “unclear exactly why” people suffering from mental health issues are more likely to be infected, says NPR. “The study controlled for certain factors, including physical risk factors and those who were having serious housing and economic difficulties – but the risk persisted.”
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
“This finding was unexpected and needs investigation,” said lead study author Dr Maxime Taquet, an academic foundation officer at Oxford. “In the meantime, having a psychiatric disorder should be added to the list of risk factors for Covid-19.”
Spotting the symptoms
Psychiatry professor Paul Harrison, who co-authored the study, suggests that while a global pandemic will cause a heightened sense of anxiety in many people, something more severe than circumstancial mental health issues lies behind the research findings.
The study was based on data covering “just the first three months” of the health crisis, Harrison told NPR. “We of course don’t know, in longer-term follow-ups, whether these risks will go on increasing - or whether once you get to three months, then the risks after you’ve had Covid really go back to the baseline risks that all of us experience.”
Experts say that symptoms to look out for in the wake of a coronavirus diagnosis include anxiety, post-traumatic stress disorder, depression and insomnia.
“We’re seeing a lot of anxiety, a lot of fear, a lot of sadness, a lot of sense of isolation,” said Lauri Pasch, a clinical psychologist at the University of California who has been working at a rehabilitation clinic for patients who’ve been hospitalised for Covid.
The new study also found that coronavirus sufferers are significantly more likely to receive a diagnosis of dementia within three months of testing positive.
However, Harrison stresses that no direct link between the coronavirus and mental health issues has been established. He notes that, for instance, some people people affected by the virus may already have been developing dementia, but were only diagnosed for that condition after seeking medical help for Covid-19 symptoms.
“It’s not at all implausible that Covid-19 might have some direct effect on your brain and your mental health,” he said. “But I think that, again, remains to be positively demonstrated.”
-
 The environmental cost of GLP-1s
The environmental cost of GLP-1sThe explainer Producing the drugs is a dirty process
-
 Nuuk becomes ground zero for Greenland’s diplomatic straits
Nuuk becomes ground zero for Greenland’s diplomatic straitsIN THE SPOTLIGHT A flurry of new consular activity in the remote Danish protectorate shows how important Greenland has become to Europeans’ anxiety about American imperialism
-
 ‘This is something that happens all too often’
‘This is something that happens all too often’Instant Opinion Opinion, comment and editorials of the day
-
 ‘Longevity fixation syndrome’: the allure of eternal youth
‘Longevity fixation syndrome’: the allure of eternal youthIn The Spotlight Obsession with beating biological clock identified as damaging new addiction
-
 A Nipah virus outbreak in India has brought back Covid-era surveillance
A Nipah virus outbreak in India has brought back Covid-era surveillanceUnder the radar The disease can spread through animals and humans
-
 A real head scratcher: how scabies returned to the UK
A real head scratcher: how scabies returned to the UKThe Explainer The ‘Victorian-era’ condition is on the rise in the UK, and experts aren’t sure why
-
 How dangerous is the ‘K’ strain super-flu?
How dangerous is the ‘K’ strain super-flu?The Explainer Surge in cases of new variant H3N2 flu in UK and around the world
-
 RFK Jr. sets his sights on linking antidepressants to mass violence
RFK Jr. sets his sights on linking antidepressants to mass violenceThe Explainer The health secretary’s crusade to Make America Healthy Again has vital mental health medications on the agenda
-
 Covid-19 mRNA vaccines could help fight cancer
Covid-19 mRNA vaccines could help fight cancerUnder the radar They boost the immune system
-
 The ‘menopause gold rush’
The ‘menopause gold rush’Under the Radar Women vulnerable to misinformation and marketing of ‘unregulated’ products
-
 The new Stratus Covid strain – and why it’s on the rise
The new Stratus Covid strain – and why it’s on the riseThe Explainer ‘No evidence’ new variant is more dangerous or that vaccines won’t work against it, say UK health experts