What is America's COVID endgame?
With cases in retreat and vaccines for children imminent, when can we breathe?


A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
America's COVID-19 case numbers are the lowest they've been since mid-summer, back when we thought the coronavirus nightmare was all but over. Vaccine approval for 5- to 11-year-olds is just days away, booster shots are available for many adults, new antiviral treatments are on the horizon, and the Biden administration's vaccine mandates are slowly but surely moving the needle on inoculating the deliberately recalcitrant minority of Americans who would rather die and kill their neighbors than get a free miracle vaccine. Despite persistently high daily death totals virtually baked in by the last month's case numbers, the situation is, objectively, better than it was two months ago.
So why doesn't it feel like we are on the verge of catharsis, as it did in April and May? Perhaps it's because things are still somewhat weird and stressful a lot of the time. Navigating daily COVID decision making and risk assessment and working around supply chain issues, labor shortages, and other ongoing disruptions is exhausting. And the sense that the situation is still not quite right is almost certainly contributing to the sour political mood dragging down President Biden's approval numbers and threatening a Democratic wipeout in next year's midterm elections.
In states with the most restrictive COVID policies, like my state of Illinois, even follow-the-science types could really use a sense of an ending. And with national public health authorities staying mum about what they would have to see to recommend a halt to most masking guidelines, people are starting to ask what the endgame is.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
First, about that weirdness: On Saturday, my wife and I took our 3-year old son, Anoush, to the magnificent Shedd Aquarium in Chicago for the first time since before the coronavirus stormed the cockpit of our lives and steered us into indefinite oblivion. And as much as I wanted to feel the rush of relief for the long-awaited return of the Before Times, it wasn't nearly the same.
Anoush bounded giddily through the aquarium in 45 minutes flat, moving frenetically from one exhibit to another. "I want to see something new," he chirped every three minutes or so, and we did. Dolphins and whales and otters and Amazonian river fish and dazzling Caribbean sea creatures filled his eyes and our hearts. But keeping his mask over his nose was a constant struggle, the crowd was denser than we would have liked, and yes, keeping my own sweaty mask plastered to my face the whole time diminished the experience. And of course, late that night Anoush came down with a cold, triggering another day-long bout of anguish that we had selfishly exposed him to the coronavirus.
This virus, am I right? It still finds ways to beat you down even when you try to avoid it, even when you feel like you've found a balance between the utterly heedless and the debilitatingly overcautious. And as someone who has done everything public health authorities have asked for close to two years now, from "two weeks to flatten the curve" and horizonless social distancing to working from home, skipping Thanksgiving and Christmas with family in 2020, getting vaccinated at the first opportunity, and then accepting the return of masking in August, I can't deny that a certain simmering discontent with the way we are living is starting to set in.
Here's one problem with the matrix of current guidance and messaging: On the one hand, official public health strategy is designed to reduce "severe illness and death" from COVID-19. That is why, for example, the official CDC guidance only recommends booster shots for a minority of the adult population, implicitly arguing that for healthy, vaccinated adults who work in "low risk" occupations and have no underlying health problems, a case of COVID is indeed no worse than the flu. If it had been up to many scientists in the Food and Drug Administration, very few Americans under 65 would get boosters at all, so thorough is their confidence in the efficacy of the vaccines.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
On the other, the lived reality that parents and employees in many industries experience is a hyper-cautious desire to prevent any and all cases, even among fully vaccinated people who are highly unlikely to fall seriously ill from infection. Many school districts now impose 10-day quarantines on perfectly healthy children who were exposed to someone with the virus, throwing hundreds of thousands of parents, at least temporarily, back into their early pandemic nightmares of around-the-clock care and work. Perhaps in a country with paid childcare and family leave and other forms of social support, this could work, but in America, these parents have nowhere to go. That dynamic, in turn, fuels panic about cases and demands for ongoing mitigation measures.
In my workplace, we teach and learn in masks, and vaccination is required to set foot on campus (with very few and stringent exceptions). We had one minor outbreak in September, which was quickly contained via a week of remote instruction, and no one infected fell seriously ill. These rules were imposed, with near-total solidarity among faculty and staff, during the worst of the late-summer Delta wave, and they will remain in place at least as long as Illinois requires universal indoor masking.
But can you really blame people for asking when we might be able to stop?
I reluctantly supported a return to masks when it was clear that the situation was spiraling out of control, but I would like, at some point, to see the bottom halves of my students' and colleagues' faces again and to resume other spontaneous kinds of socializing that remain off the table. It's not clear how much longer masking regimes can hold without resentment building to unsustainable levels. Once all parents who want to vaccinate their children can do so, likely by sometime in January or February, what possible justification could there be to keep restrictions in place for vaccinated people, especially when the federal government refuses to drop its last remaining hammers on anti-vaxxers, like instituting a vaccine mandate for air travel?
To be sure, the coming endemicity of COVID-19 will pose an ongoing public health challenge. Flu season was always an underappreciated problem, and now we will have two different potentially deadly viruses circulating globally. But instead of making permanent and unwanted changes to society, like long periods of masking or remote work every winter as some are floating, why not throw a few trillion dollars at new flu vaccines and treatments, ventilation improvements, and sick leave policies that give American workers the freedom to take time off when they are unwell? Why not invest in a moonshot program to fight immune disorders? Why not scale up our health-care infrastructure to meet the coming curves?
Whatever path we ultimately choose, the American people need to be told when they can fly, take public transit, go to school, visit the grocery store, or attend indoor cultural events without masks on their faces and fear in their souls. Yes, many red states are defying current national guidelines and will continue to do so no matter what. The rest of us are looking for the off-ramp. Are we shooting for a specific vaccination rate? Will it be about community transmission numbers? Hospitalization figures?
The tantalizing promise of a return to ordinary life is the only thing that got many people through last winter. As our second pandemic winter looms, we need to know when that promise will finally be realized.
David Faris is a professor of political science at Roosevelt University and the author of "It's Time to Fight Dirty: How Democrats Can Build a Lasting Majority in American Politics." He's a frequent contributor to Newsweek and Slate, and his work has appeared in The Washington Post, The New Republic and The Nation, among others.
-
 How to Get to Heaven from Belfast: a ‘highly entertaining ride’
How to Get to Heaven from Belfast: a ‘highly entertaining ride’The Week Recommends Mystery-comedy from the creator of Derry Girls should be ‘your new binge-watch’
-
 The 8 best TV shows of the 1960s
The 8 best TV shows of the 1960sThe standout shows of this decade take viewers from outer space to the Wild West
-
 Microdramas are booming
Microdramas are boomingUnder the radar Scroll to watch a whole movie
-
 A Nipah virus outbreak in India has brought back Covid-era surveillance
A Nipah virus outbreak in India has brought back Covid-era surveillanceUnder the radar The disease can spread through animals and humans
-
 Covid-19 mRNA vaccines could help fight cancer
Covid-19 mRNA vaccines could help fight cancerUnder the radar They boost the immune system
-
 The new Stratus Covid strain – and why it’s on the rise
The new Stratus Covid strain – and why it’s on the riseThe Explainer ‘No evidence’ new variant is more dangerous or that vaccines won’t work against it, say UK health experts
-
 RFK Jr. vaccine panel advises restricting MMRV shot
RFK Jr. vaccine panel advises restricting MMRV shotSpeed Read The committee voted to restrict access to a childhood vaccine against chickenpox
-
 RFK Jr. scraps Covid shots for pregnant women, kids
RFK Jr. scraps Covid shots for pregnant women, kidsSpeed Read The Health Secretary announced a policy change without informing CDC officials
-
 New FDA chiefs limit Covid-19 shots to elderly, sick
New FDA chiefs limit Covid-19 shots to elderly, sickspeed read The FDA set stricter approval standards for booster shots
-
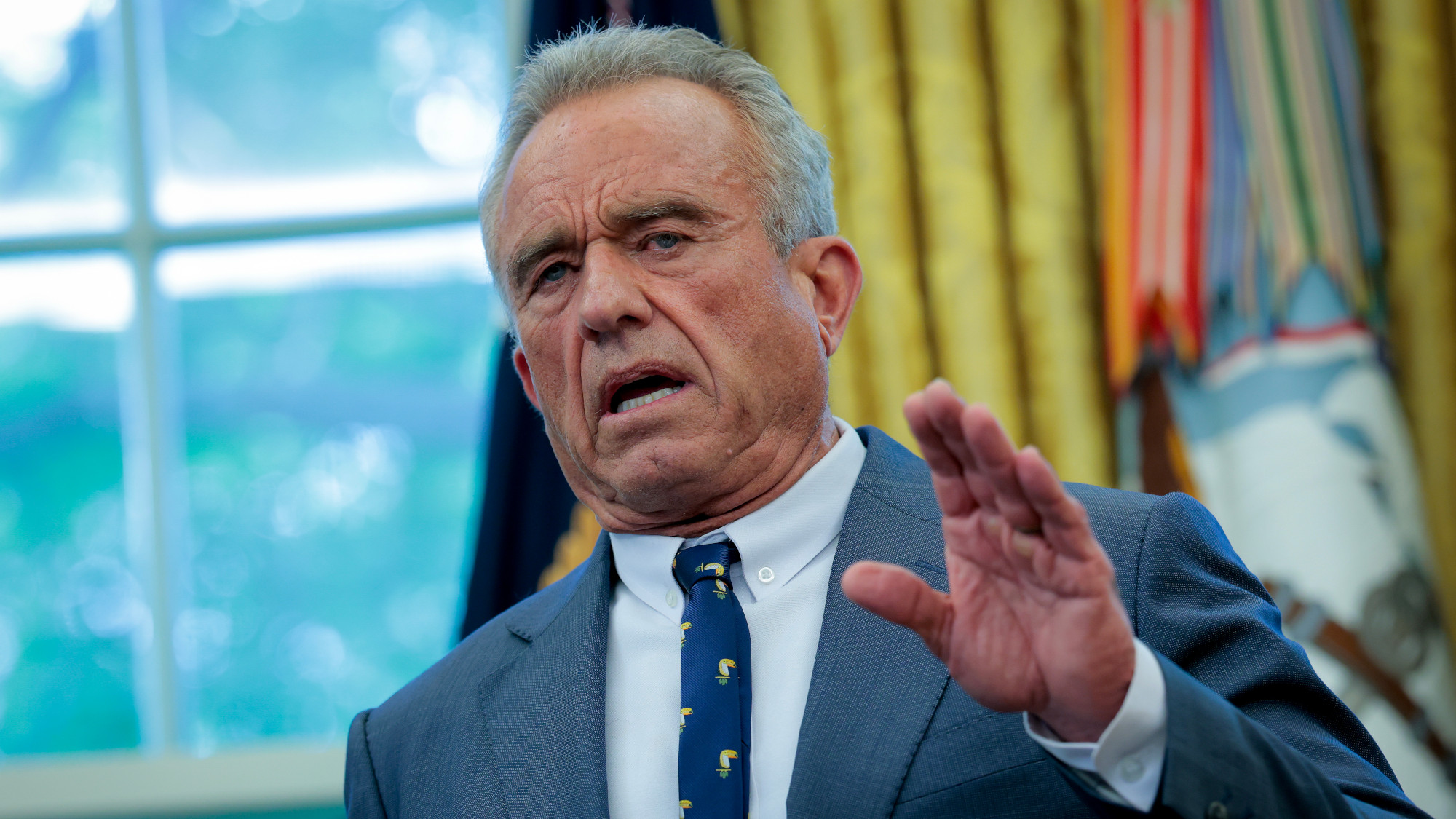 RFK Jr.: A new plan for sabotaging vaccines
RFK Jr.: A new plan for sabotaging vaccinesFeature The Health Secretary announced changes to vaccine testing and asks Americans to 'do your own research'
-
 Five years on: How Covid changed everything
Five years on: How Covid changed everythingFeature We seem to have collectively forgotten Covid’s horrors, but they have completely reshaped politics
