Solving COVID: August 5, 2020
Novavax vaccine produces strong antibody response, state governors team up to expand testing, and more
- 1. Novavax announces promising early coronavirus vaccine trials
- 2. Seven states are teaming up to expand COVID-19 testing
- 3. Eli Lilly testing antibody drug to stem outbreaks in nursing homes
- 4. State attorneys general seek to lower Gilead's high remdesivir prices
- 5. Public transportation may not be a major source of coronavirus transmission, studies suggest
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
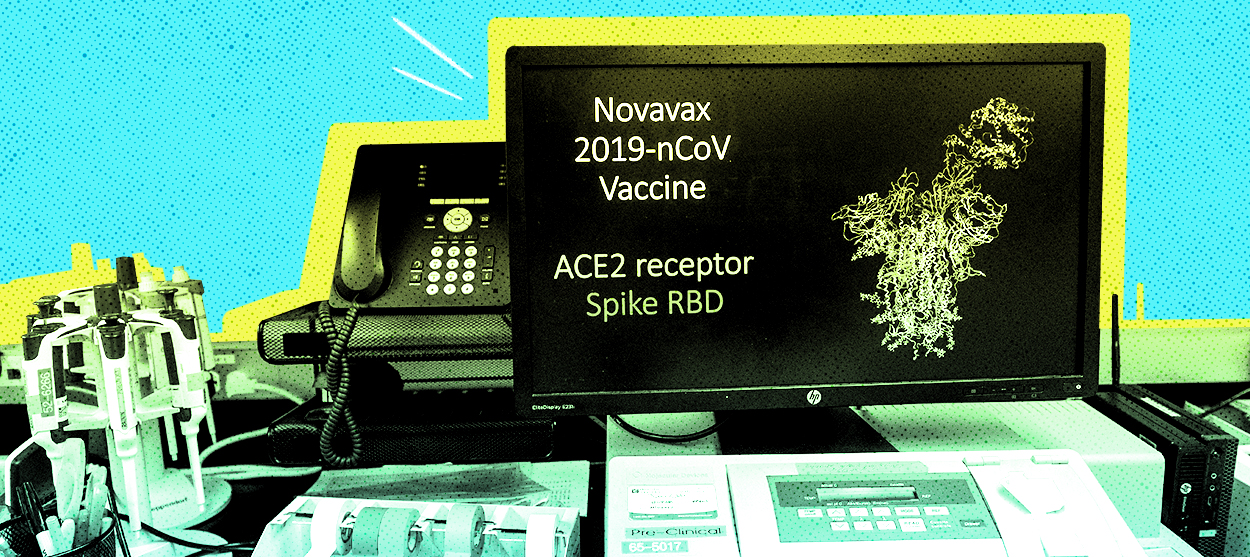
1. Novavax announces promising early coronavirus vaccine trials
Novavax on Tuesday announced encouraging results in two preliminary trials of its experimental coronavirus vaccine. The company reached a $1.6 billion deal with the federal government to develop the vaccine, even though it has never brought a vaccine to market before. In one study, the drug appeared to protect monkeys from infection. In the other, 56 human volunteers given the potential vaccine produced high levels of antibodies to fight the virus, without dangerous side effects. "This is the first one I'm looking at and saying, 'Yeah, I'd take that,'" said Dr. John Moore, a Weill Cornell Medicine virologist who was not involved in the studies. Novavax has said it can produce 100 million doses by the beginning of 2021. The company is one of several racing to develop a vaccine.
2. Seven states are teaming up to expand COVID-19 testing
The governors of Maryland, Louisiana, Massachusetts, Michigan, Ohio, Virginia, and North Carolina have announced an interstate compact "to expand the use of rapid point-of-care antigen tests" during the coronavirus pandemic. The bipartisan group of governors is in talks to buy 500,000 antigen tests for each state. "By banding together, the states are demonstrating to private manufacturers that there is significant demand to scale up the production of these tests, which deliver results in 15-20 minutes," the announcement said, touting this as the first such interstate testing agreement during the pandemic. The compact was negotiated by Maryland Gov. Larry Hogan (R), who on Tuesday said "we will be working to bring additional states, cities, and local governments on board as this initiative moves forward."
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
Gov. Larry Hogan The Washington Post
3. Eli Lilly testing antibody drug to stem outbreaks in nursing homes
Eli Lilly & Co. has started a Phase 3 trial of its experimental antibody-based COVID-19 drug in nursing homes and other long-term care facilities, testing whether the drug reduces the infection rate at facilities where residents or staff have recently tested positive for the new coronavirus. The study, which seeks to enroll 2,400 test subjects, involves Eli Lilly driving specially modified RVs to newly infected nursing homes and injecting its COVID-19 drug, code-named LY-CoV555, in volunteers, The Wall Street Journal reports. Nursing homes have been especially susceptible to deadly COVID-19 outbreaks. The company said its drug may get government approval by the end of 2020. If Eli Lilly's drug or another like it proves safe and effective, public health experts say it might serve as a bridge until a vaccine is available.
4. State attorneys general seek to lower Gilead's high remdesivir prices
The antiviral drug remdesivir's effectiveness at combating the coronavirus has been one of the biggest breakthroughs since the pandemic began. The catch is that the Gilead treatment is expensive and in short supply. A bipartisan group of state attorneys general are looking to the federal government to step in and change that. In a letter to the heads of the Department of Health and Human Services, the National Institutes of Health, and the Food and Drug Administration, 31 attorneys general asked the agencies to exercise march-in rights granted to them by the 1980 Bayh-Dole Act to increase the supply of the drug and lower the price so it becomes more accessible to Americans. The bill allows federal agencies to retain patent rights for drugs developed from federal funds if the manufacturer fails to achieve a reasonable price or "alleviate health or safety needs" of consumers.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
5. Public transportation may not be a major source of coronavirus transmission, studies suggest
In several major cities where ridership on public transportation has rebounded, there haven't been any coronavirus outbreaks linked to subways, buses, or commuter railways, The New York Times reports. In Paris, contact tracers have not found public transportation to be linked to any of the city's 386 coronavirus clusters between early May and mid-July. The same goes for Tokyo's famously busy system, and an Austrian study couldn't trace any outbreaks to public transportation in the country, either. The findings are encouraging, but come with some caveats: Ridership is still short of pre-pandemic levels in most places, and those cities where passengers are taking public transportation in more significant numbers have mandated masks, disinfected trains and buses, and ramped up service to avoid overcrowding. That will likely be the blueprint for many cities going forward, at least while the pandemic continues. A lot remains unknown, but the Times reports that riding public transportation probably falls somewhere in between walking outdoors and dining indoors on the safety scale.