Coronavirus: will the Oxford Covid vaccine be the true game-changer?
Latest trial results show the university’s jab is up to 90% effective
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
A coronavirus vaccine developed by the University of Oxford is between 70% and 90% effective at preventing people from getting Covid-19, according to preliminary data.
Results from Phase 3 trials show that the vaccine, made in partnership with Cambridge-based company AstraZeneca, is 70.4% effective on average. But researchers say that when administered at a half dose and then a full dose, rather than two full doses, the vaccine can be up to 90% effective.
The study, which involved more than 24,000 volunteers, showed there were “no serious cases among those who received the vaccine, including no hospitalisations”, The Telegraph reports.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
At what stage of development is the Oxford vaccine?
The Oxford University vaccine has long been a front runner in the contest to find a coronavirus jab.
In early September, trials of the vaccine resumed after being briefly paused as a result of a reported side effect in a patient in the UK. The jab is in ongoing Phase 3 testing that has involved a total of around 30,000 participants in the US, UK, Brazil and South Africa.
The newly published results show that “there were 30 cases of Covid in people who had two doses of the vaccine and 101 cases in people who received a dummy injection”, the BBC reports. The researchers say this works out as equivalent to 70% protection.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
When volunteers were given two high doses, the protection rate was 62%, but this figure rose to 90% among those given a low dose followed by a high one. “It’s not clear why there is a difference,” the broadcaster says.
Although very encouraging, the Oxford results fall short of those for jabs developed by US pharmaceuticals giant Pfizer and Massachusetts-based Moderna, both of which have been show to offer up to 95% protection in late-stage trials.
However, the Oxford vaccine is far cheaper, and is easier to store and transport, than the two rival versions.
The UK has so far purchased 40 million doses of the vaccine developed by Pfizer, and has also rushed to reserve five million of Moderna’s candidate.
But No. 10 has even more hopes invested in the Oxford vaccine, of which the UK has reserved 100 million doses.
How does the jab differ from the other candidates?
While the Oxford vaccine – called ChAdOx1 nCoV-19 – “uses a different technology from the Moderna jab, the two vaccines both rely on stimulating cells to produce a specific protein, which in turn triggers an immune response”, The Guardian reports.
But unlike the Oxford jab, those developed by Modena and Pfzier use messenger ribonucleic acid, also known as messenger RNA, or mRNA.
Conventional vaccines are produced using weakened forms of a virus, but mRNAs use only the genetic code of the virus. In the Covid vaccines, the mRNA carries instructions for making the spike protein that protrudes from the outside of the coronavirus cell.
Once injected, the vaccine causes “protein-making machinery within the human cells to churn out this spike protein”, prompting the immune system to go into defence mode, the paper explains.
By contrast, the Oxford version is a conventional vaccine, using a harmless, weakened version of a common virus that causes colds in chimpanzees. Researchers have previously used this technology to produce vaccines against pathogens including flu, Zika and Middle East Respiratory Syndrome (Mers).
The Oxford team are now using the “harmless chimp cold virus to deliver genetic information from the coronavirus to human cells to trigger the production of the spike protein” that kick-starts the immune response, says The Guardian.
In a major boost for their version, the Oxford vaccine can be stored at fridge temperature, which “means it can be distributed to every corner of the world, unlike the Pfizer/BioNTech and Moderna vaccines, which need to be stored at much colder temperatures”, the BBC reports.
And AstraZeneca has said it is preparing to make three billion doses worldwide at a price of around £3 - a price tag that is considerably less than those for Pfizer’s (£15) or Moderna’s (£25) vaccines.
So will it end the pandemic?
Professor Andrew Pollard, director of the Oxford Vaccine Group, told The Guardian that “the positive results from the other developers means it is likely that there will be multiple vaccines on target, which is great news for the world”.
But concerns persist over how long the vaccine protection will last.
Since the Oxford jab “uses a live chimpanzee adenovirus to transport elements of Sars-Cov-2 into humans, it’s expected people will develop immunity to the viral vector, preventing the vaccine from being used for future top-ups”, The Independent reports.
“For a scenario where the Oxford vaccine gets rolled out across the UK, that might give people protection for six months to a year,” Professor Robin Shattock, who is leading a separate team of vaccine researchers at Imperial College London, told the paper. “But you then need something to come back and reboost people.”
Shattock believes that his vaccine could be used as a regular booster for maintaining immunity. And that could offer “a permanent route out of the pandemic”, The Independent suggests.
In the meantime, the Oxford vaccine needs to be approved by regulators, “who will assess the vaccine's safety, effectiveness, and that it is manufactured to high standard,” adds the BBC. “This process will happen in the coming weeks.”
-
 How the FCC’s ‘equal time’ rule works
How the FCC’s ‘equal time’ rule worksIn the Spotlight The law is at the heart of the Colbert-CBS conflict
-
 What is the endgame in the DHS shutdown?
What is the endgame in the DHS shutdown?Today’s Big Question Democrats want to rein in ICE’s immigration crackdown
-
 ‘Poor time management isn’t just an inconvenience’
‘Poor time management isn’t just an inconvenience’Instant Opinion Opinion, comment and editorials of the day
-
 A Nipah virus outbreak in India has brought back Covid-era surveillance
A Nipah virus outbreak in India has brought back Covid-era surveillanceUnder the radar The disease can spread through animals and humans
-
 Trump HHS slashes advised child vaccinations
Trump HHS slashes advised child vaccinationsSpeed Read In a widely condemned move, the CDC will now recommend that children get vaccinated against 11 communicable diseases, not 17
-
 A fentanyl vaccine may be on the horizon
A fentanyl vaccine may be on the horizonUnder the radar Taking a serious jab at the opioid epidemic
-
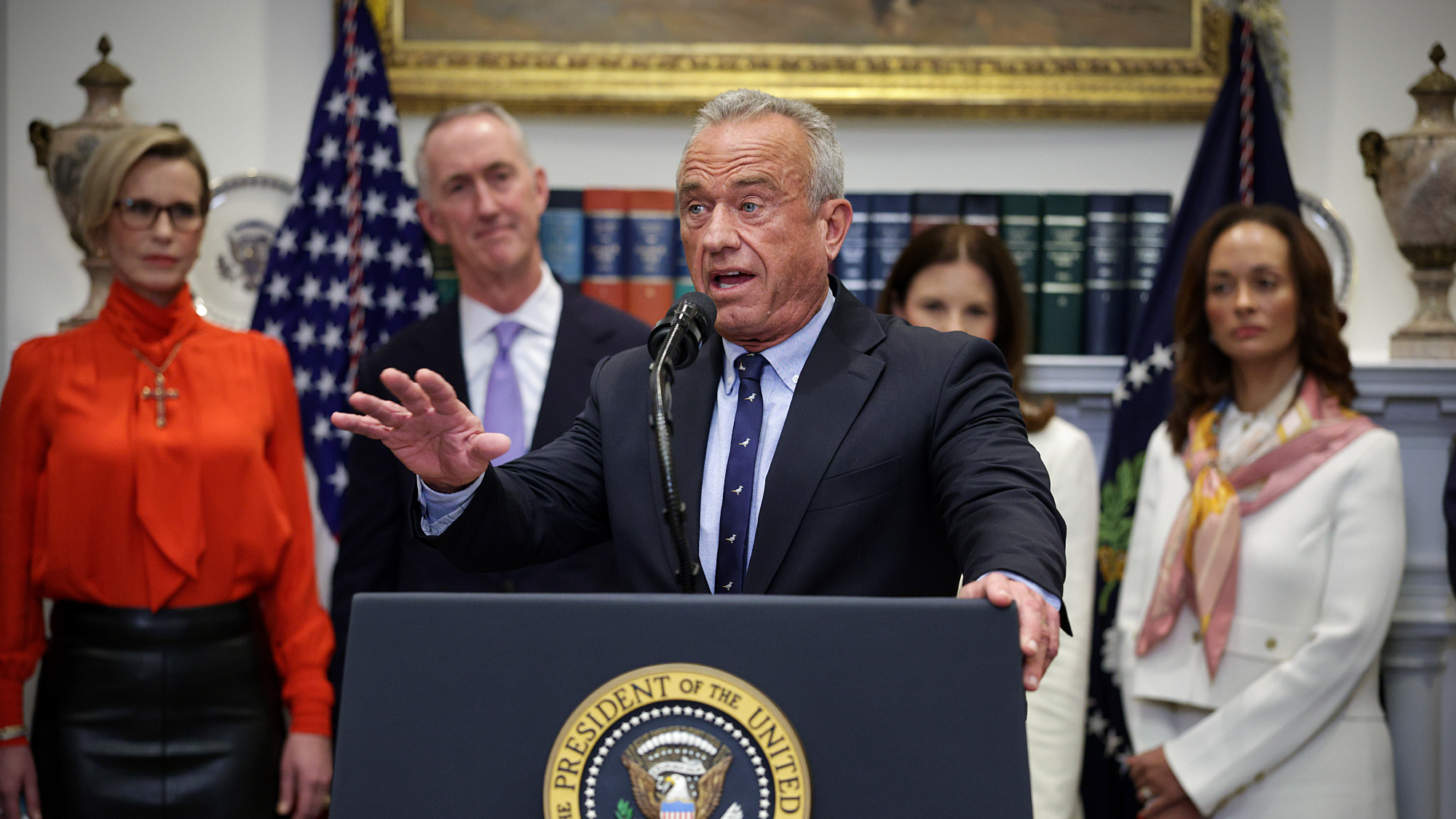
 Health: Will Kennedy dismantle U.S. immunization policy?
Health: Will Kennedy dismantle U.S. immunization policy?Feature ‘America’s vaccine playbook is being rewritten by people who don’t believe in them’
-
 How dangerous is the ‘K’ strain super-flu?
How dangerous is the ‘K’ strain super-flu?The Explainer Surge in cases of new variant H3N2 flu in UK and around the world
-
 Vaccine critic quietly named CDC’s No. 2 official
Vaccine critic quietly named CDC’s No. 2 officialSpeed Read Dr. Ralph Abraham joins another prominent vaccine critic, HHS Secretary Robert F. Kennedy Jr.
-
 This flu season could be worse than usual
This flu season could be worse than usualIn the spotlight A new subvariant is infecting several countries
-
 Covid-19 mRNA vaccines could help fight cancer
Covid-19 mRNA vaccines could help fight cancerUnder the radar They boost the immune system