Coronavirus: three things you need to know about the Covid-19 vaccine
An immunologist answers the most common questions about the jab

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Tracy Hussell, professor of inflammatory disease at the University of Manchester, answers the questions you need to know about the rollout of the coronavirus vaccine.
If we are ever to return to some semblance of normality, then the world’s population needs to be immune to SARS-CoV-2, the virus that causes Covid-19.
But with so many different vaccines in production, questions are undoubtedly going to be raised, such as can I still have a vaccine if I have been involved in a trial testing other versions? And, what if I’ve already had Covid – do I still need a vaccine? A basic understanding of immunology can answer all these questions.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
All Covid vaccines try to generate an immune response to proteins the virus needs to enter your cells. Whether this is by using a harmless virus carrying the protein that mimics SARS-CoV-2 but doesn’t replicate, or by using the genetic code for those proteins (a messenger RNA), the outcome is the same.
The protein critical to stopping SARS-CoV-2 is displayed, recognised by the immune system, and the body produces antibodies and T cells that are then ready to stop future infection.
Is it OK to have a different second dose?
A booster vaccination enhances the quality of the immune response and sends a reminder about the virus. It doesn’t matter if the vaccine used to prime the immune system is different from the one used to boost, as long as they both contain the critical viral protein.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
Booster vaccinations are common, and the time interval between them varies. For example, a booster for tetanus is advised every ten years whereas vaccines for hepatitis A or measles are one-shot wonders – a booster is not needed.
Only by studying the immune response in people who have been vaccinated, will we be able to tell when and if further booster vaccinations are needed. This will be determined by measuring SARS-CoV-2 specific antibody and T cell responses in a sample of blood.
It is possible that certain groups, such as older people, might need a different booster strategy – and this will take time to work out.
What if I’ve already had a trial vaccine?
If you’ve taken part in a Covid vaccine trial, it could give you a head start on the prime/boost approach, and you could reach the required immunity threshold quicker. Alternatively, your trial vaccination may have been so effective that the non-trial version of the vaccine isn’t necessary.
It is important for vaccine developers to follow up people who have had the vaccine to see how their immune system has reacted and whether or not the vaccine gave them immunity.
This follow up should be conducted over a long period and encompass different sections of the population: young, old, different ethnic groups, and patients on drugs that dampen the immune system (such as chemotherapy).
What if I’ve had Covid?
Even if you have recovered from Covid-19, you can still benefit from vaccination. There is evidence in hospitalised patients that the infection was so overwhelming that the immune response became exhausted and so immune memory to the virus was not created efficiently.
Also, if you had a very mild infection, your immune system may not have reached the point of laying down immune memory. So vaccination could be beneficial, regardless of whether you experienced severe or mild disease.
Though vaccination is a choice, don’t forget that vaccines have been around a long time and have saved more lives than any other medicine. The risk of getting Covid and its awful and often long-term side-effects outweigh any theoretical risk of a vaccine.
Tracy Hussell, professor of inflammatory disease at the University of Manchester.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
-
 The environmental cost of GLP-1s
The environmental cost of GLP-1sThe explainer Producing the drugs is a dirty process
-
 Greenland’s capital becomes ground zero for the country’s diplomatic straits
Greenland’s capital becomes ground zero for the country’s diplomatic straitsIN THE SPOTLIGHT A flurry of new consular activity in Nuuk shows how important Greenland has become to Europeans’ anxiety about American imperialism
-
 ‘This is something that happens all too often’
‘This is something that happens all too often’Instant Opinion Opinion, comment and editorials of the day
-
 A Nipah virus outbreak in India has brought back Covid-era surveillance
A Nipah virus outbreak in India has brought back Covid-era surveillanceUnder the radar The disease can spread through animals and humans
-
 Covid-19 mRNA vaccines could help fight cancer
Covid-19 mRNA vaccines could help fight cancerUnder the radar They boost the immune system
-
 The new Stratus Covid strain – and why it’s on the rise
The new Stratus Covid strain – and why it’s on the riseThe Explainer ‘No evidence’ new variant is more dangerous or that vaccines won’t work against it, say UK health experts
-
 RFK Jr. vaccine panel advises restricting MMRV shot
RFK Jr. vaccine panel advises restricting MMRV shotSpeed Read The committee voted to restrict access to a childhood vaccine against chickenpox
-
 RFK Jr. scraps Covid shots for pregnant women, kids
RFK Jr. scraps Covid shots for pregnant women, kidsSpeed Read The Health Secretary announced a policy change without informing CDC officials
-
 New FDA chiefs limit Covid-19 shots to elderly, sick
New FDA chiefs limit Covid-19 shots to elderly, sickspeed read The FDA set stricter approval standards for booster shots
-
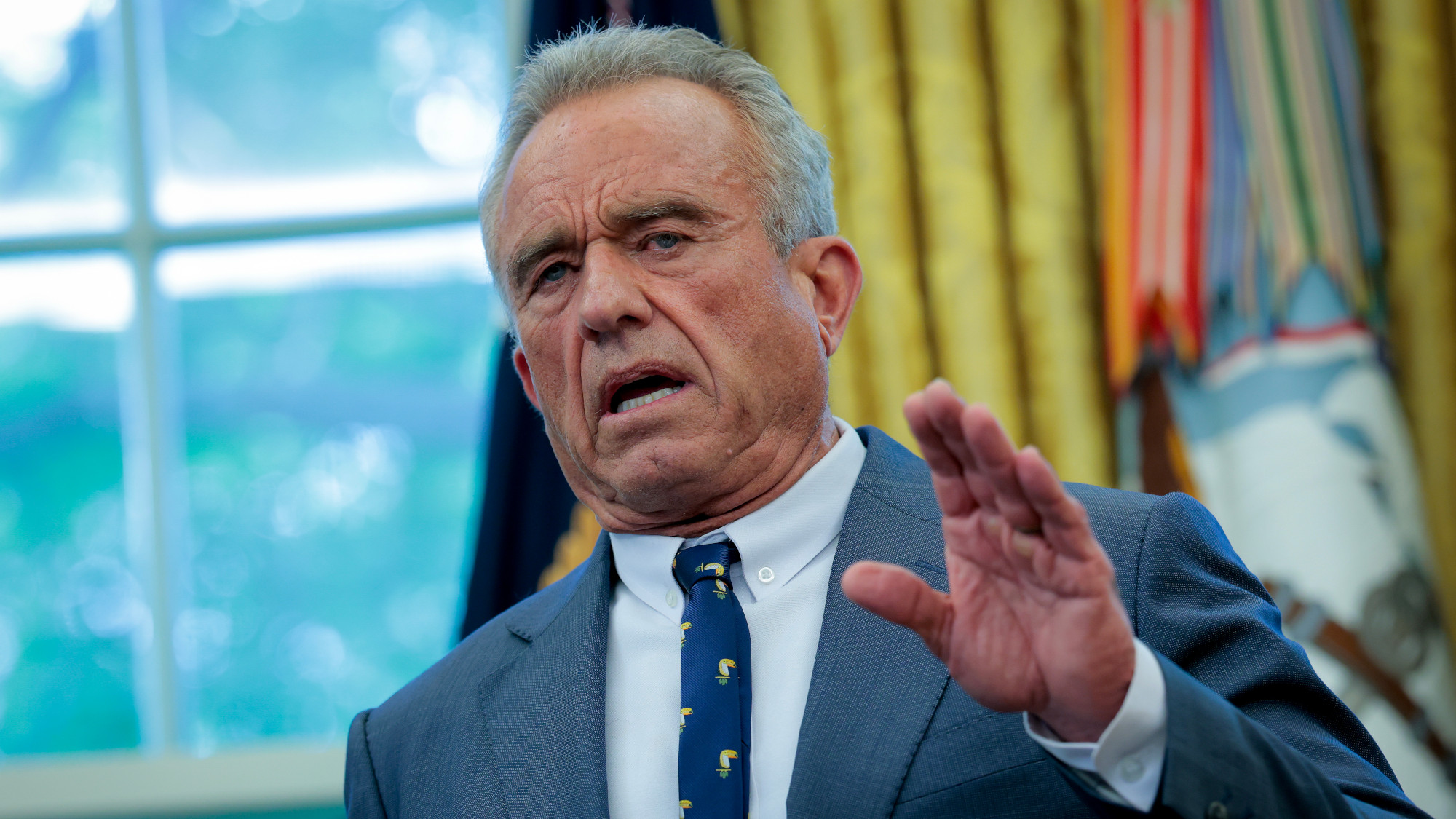 RFK Jr.: A new plan for sabotaging vaccines
RFK Jr.: A new plan for sabotaging vaccinesFeature The Health Secretary announced changes to vaccine testing and asks Americans to 'do your own research'
-
 Five years on: How Covid changed everything
Five years on: How Covid changed everythingFeature We seem to have collectively forgotten Covid’s horrors, but they have completely reshaped politics