How Oxford scientists developed a Covid-19 vaccine in record time
Experts involved in the inoculation race explain how the jab was developed

A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Tonia Thomas, vaccine knowledge project manager at the University of Oxford and Rachel Colin-Jones, visiting academic at Oxford University’s Centre for Clinical Vaccinology and Tropical Medicine, on how the first vaccine developed in the UK was produced.
The pandemic is only a year old, but we already have multiple vaccines available to fight Covid-19 – including the vaccine developed by the team we’re part of at the University of Oxford.
With our partner AstraZeneca, we have submitted both interim efficacy data and safety data for the vaccine to regulators across the world for independent scrutiny and approval. So far the vaccine has been approved for emergency use in the UK, India, Morocco, Argentina and El Salvador.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
As well as being great news for getting us back to normal, this represents a phenomenal scientific achievement. Typically, developing a vaccine takes decades – but we have several available for Covid-19 after just 12 months. Here’s how we managed this for the Oxford vaccine.
A head-start on development
Our vaccine works by delivering the genetic sequence of the SARS-CoV-2 spike protein to the body’s cells (the spike proteins are the distinctive structures that “crown” the coronavirus’s surface).
The body’s cells read this genetic code and start producing copies of the spike protein, and the immune system then mounts a response against these proteins and remembers them. This means that if SARS-CoV-2 later enters the body, its spike proteins will immediately flag it to the immune system for destruction.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
This may sound complicated, but when the pandemic arrived, we had a head start, as we had already developed a delivery method – or “platform” – for our vaccine and had been testing it for other diseases for almost ten years. Known as the ChAdOx1 viral vector technology, this platform was created by modifying a harmless adenovirus that causes the common cold in chimpanzees.
ChAdOx1 was chosen as it can generate a strong immune response and is not a replicating virus, so cannot cause an infection. It had already been used safely in thousands of subjects in clinical trials of vaccines for other diseases including Middle Eastern respiratory syndrome (Mers), which is caused by another type of coronavirus.
Our ongoing research into ChAdOx1 was part of preparing for “Disease X”, one of eight diseases prioritised for research by the World Health Organization (WHO) due to the risk they pose to public health. Covid-19 has since been added to this list.
Disease X is a placeholder name that highlights that the next serious epidemic could be caused by a pathogen as yet unknown to scientists, which is what happened with the coronavirus.
Having an already developed platform ready meant that testing of the vaccine could begin quickly. University of Oxford
Once researchers in China had mapped the genetic sequence of the coronavirus, we were able to quickly produce our Covid-19 vaccine by combining the ChAdOx1 vector with the genetic sequence of the SARS-CoV-2 spike protein.
The preparation for Disease X ultimately allowed our research team to move straight into testing our vaccine in animals in early 2020, and then to combine the data from these tests with data we had already gathered in previous trials using ChAdOx1, to show that what we were developing worked.
Making human trials more efficient
With good data from our animal studies, we were ready to move onto clinical trials – essentially a series of tests to show that a treatment is safe and effective in humans.
Vaccine trials are typically split into three phases. Phase 1 assesses the safety of a vaccine and how well it is tolerated, as well as the immune response. Phase 2 involves testing on a larger, more diverse group of people and is used to identify the optimal dose and schedule.
Phase 3 then aims to test the safety and efficacy of a vaccine in a large group of people, often in multiple locations. This is usually assessed by monitoring how many cases of the disease are seen in a group that gets the vaccine versus a group that doesn’t.
Ordinarily, the different trial phases are run separately, often with time between them for preparing protocols and funding applications, then seeking ethical and regulatory approvals. But for our vaccine, we undertook combined phase 1 and 2 and phase 2 and 3 trials to speed up the development process.
This doesn’t mean that any of the required steps were missed out, but rather that we could launch the next stage of the trial as soon as we had collected enough data from the previous phase and had it reviewed by the independent Data Safety Monitoring Board.
Moving quickly but safely
Some people have questioned the speed of vaccine development during the pandemic. However, the Oxford Covid-19 vaccine trial – which is still ongoing – is undergoing the same intense scrutiny as other vaccine trials. Interim analysis has shown that the vaccine is safe and effective, but the final stages of its phase 3 trial are still being completed.
Throughout, all participants are being closely monitored, and a report is made about anyone who has a medically significant illness or is hospitalised, for whatever cause, even a broken leg. If any of these events is thought to be possibly related to the vaccine, an independent review takes place to carefully assess the medical information.
While this happens, vaccinations are paused. They’re then restarted once the review is complete and it is considered safe to continue.
All told, the vaccine will have been tested on almost five times as many volunteers as is usually required for licensing a vaccine. By the end of the trials we’re running, 24,000 people will have taken part in four countries and another 30,000 in trials run by our partners.
Testing in different populations is crucial, as any vaccine developed for Covid-19 is likely to be deployed to a large number of people worldwide.
Tonia Thomas, vaccine knowledge project manager at the University of Oxford, and Rachel Colin-Jones, visiting academic at Oxford University’s Centre for Clinical Vaccinology and Tropical Medicine.
This article is republished from The Conversation under a Creative Commons license. Read the original article.
-
 Why is the Trump administration talking about ‘Western civilization’?
Why is the Trump administration talking about ‘Western civilization’?Talking Points Rubio says Europe, US bonded by religion and ancestry
-
 Quentin Deranque: a student’s death energizes the French far right
Quentin Deranque: a student’s death energizes the French far rightIN THE SPOTLIGHT Reactions to the violent killing of an ultraconservative activist offer a glimpse at the culture wars roiling France ahead of next year’s elections
-
 Secured vs. unsecured loans: how do they differ and which is better?
Secured vs. unsecured loans: how do they differ and which is better?the explainer They are distinguished by the level of risk and the inclusion of collateral
-
 A Nipah virus outbreak in India has brought back Covid-era surveillance
A Nipah virus outbreak in India has brought back Covid-era surveillanceUnder the radar The disease can spread through animals and humans
-
 Covid-19 mRNA vaccines could help fight cancer
Covid-19 mRNA vaccines could help fight cancerUnder the radar They boost the immune system
-
 The new Stratus Covid strain – and why it’s on the rise
The new Stratus Covid strain – and why it’s on the riseThe Explainer ‘No evidence’ new variant is more dangerous or that vaccines won’t work against it, say UK health experts
-
 RFK Jr. vaccine panel advises restricting MMRV shot
RFK Jr. vaccine panel advises restricting MMRV shotSpeed Read The committee voted to restrict access to a childhood vaccine against chickenpox
-
 RFK Jr. scraps Covid shots for pregnant women, kids
RFK Jr. scraps Covid shots for pregnant women, kidsSpeed Read The Health Secretary announced a policy change without informing CDC officials
-
 New FDA chiefs limit Covid-19 shots to elderly, sick
New FDA chiefs limit Covid-19 shots to elderly, sickspeed read The FDA set stricter approval standards for booster shots
-
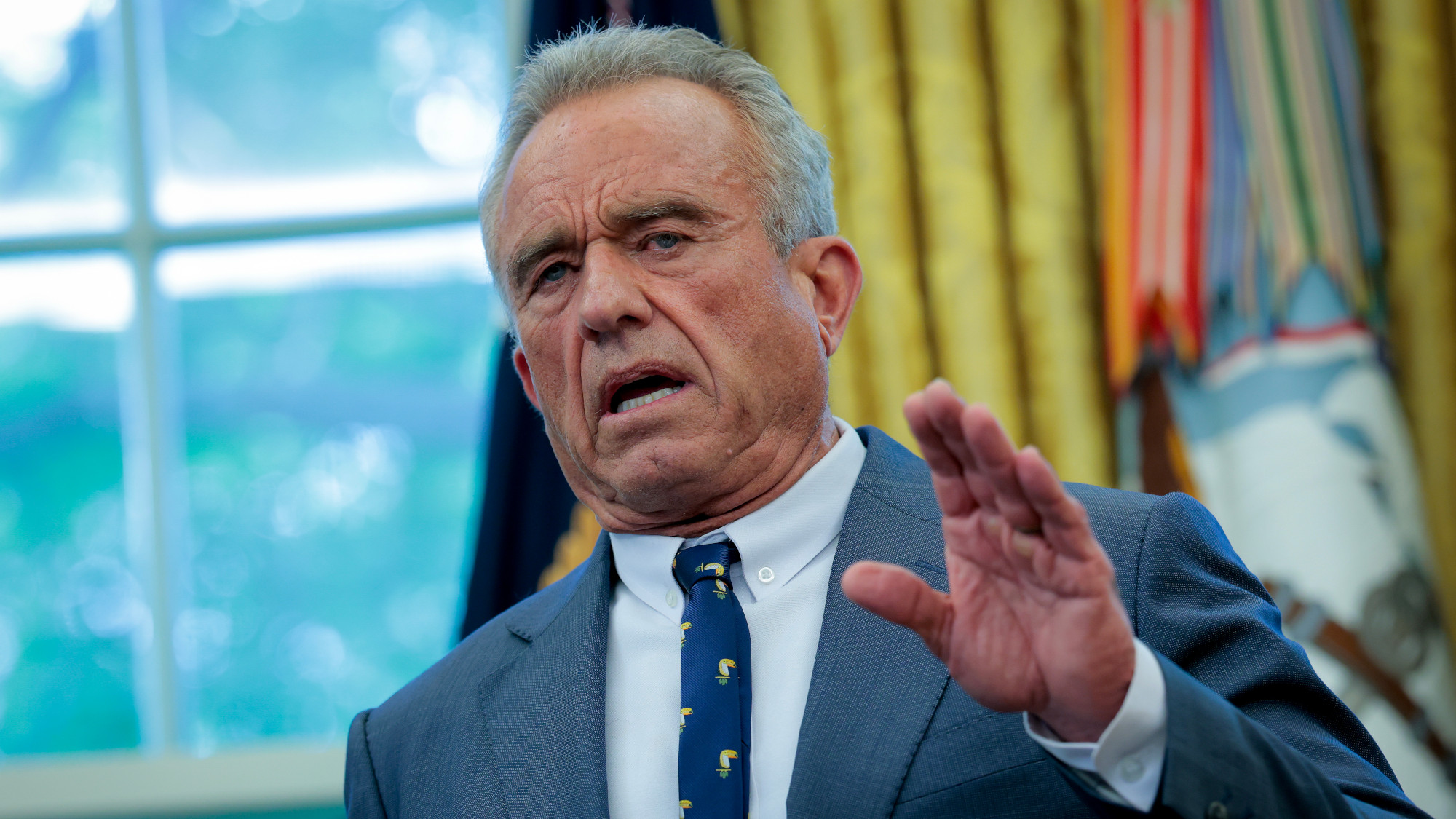 RFK Jr.: A new plan for sabotaging vaccines
RFK Jr.: A new plan for sabotaging vaccinesFeature The Health Secretary announced changes to vaccine testing and asks Americans to 'do your own research'
-
 Five years on: How Covid changed everything
Five years on: How Covid changed everythingFeature We seem to have collectively forgotten Covid’s horrors, but they have completely reshaped politics