The race for a coronavirus vaccine
Researchers are working frantically on a shot that would immunize people against COVID-19. Why does it take so long?
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
You are now subscribed
Your newsletter sign-up was successful
Researchers are working frantically on a shot that would immunize people against Covid-19. Why does it take so long? Here's everything you need to know:
Is a vaccine close?
Despite the global competition to develop a coronavirus vaccine, experts agree one won't be available for at least 12 to 18 months. The race kicked off Jan. 10, when Chinese scientists published the complete 30,000-letter genetic code of SARS-CoV-2, the novel coronavirus that causes COVID-19. That allowed scientists to make synthetic versions of the virus rather than waiting for sample shipments, and roughly 80 pharma giants, small labs, and government entities began chasing a cure. Moderna, a biotech startup in Cambridge, Massachusetts, produced a vaccine candidate that was injected into the arm of a 43-year-old Seattle mother in mid-March, smashing the world record for fastest human testing. Several other labs have since launched clinical trials. President Trump pledged to "slash red tape" slowing development, but scientists say it's not bureaucracy or pointless rules that make his request for a vaccine by summertime impossible.
The Week
Escape your echo chamber. Get the facts behind the news, plus analysis from multiple perspectives.

Sign up for The Week's Free Newsletters
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
From our morning news briefing to a weekly Good News Newsletter, get the best of The Week delivered directly to your inbox.
What's the holdup?
Before injecting a vaccine into millions of people, scientists need to conduct tests to prove that it actually protects against a specific pathogen and doesn't have serious side effects. Under normal circumstances, a vaccine can take a decade to get FDA approval. Coronavirus research is racing along, thanks largely to the Coalition for Epidemic Preparedness Innovations (CEPI), a Norway-based organization founded in 2017 to help labs like Moderna plan for "prototype" pathogens. Yet although scientists are desperate to save lives, cutting corners could have treacherous consequences. (Extremely ill patients can get unproven treatments under "compassionate use" exceptions, but vaccines are administered to people before they get sick.) A vaccine for swine flu in 1976 gave hundreds of people a rare nerve disorder, and a vaccine for H1N1 bird flu in 2009 caused some Europeans to develop narcolepsy. Some failed vaccines have made recipients more vulnerable to the disease. A candidate vaccine for SARS was abandoned after it made mice more likely to die.
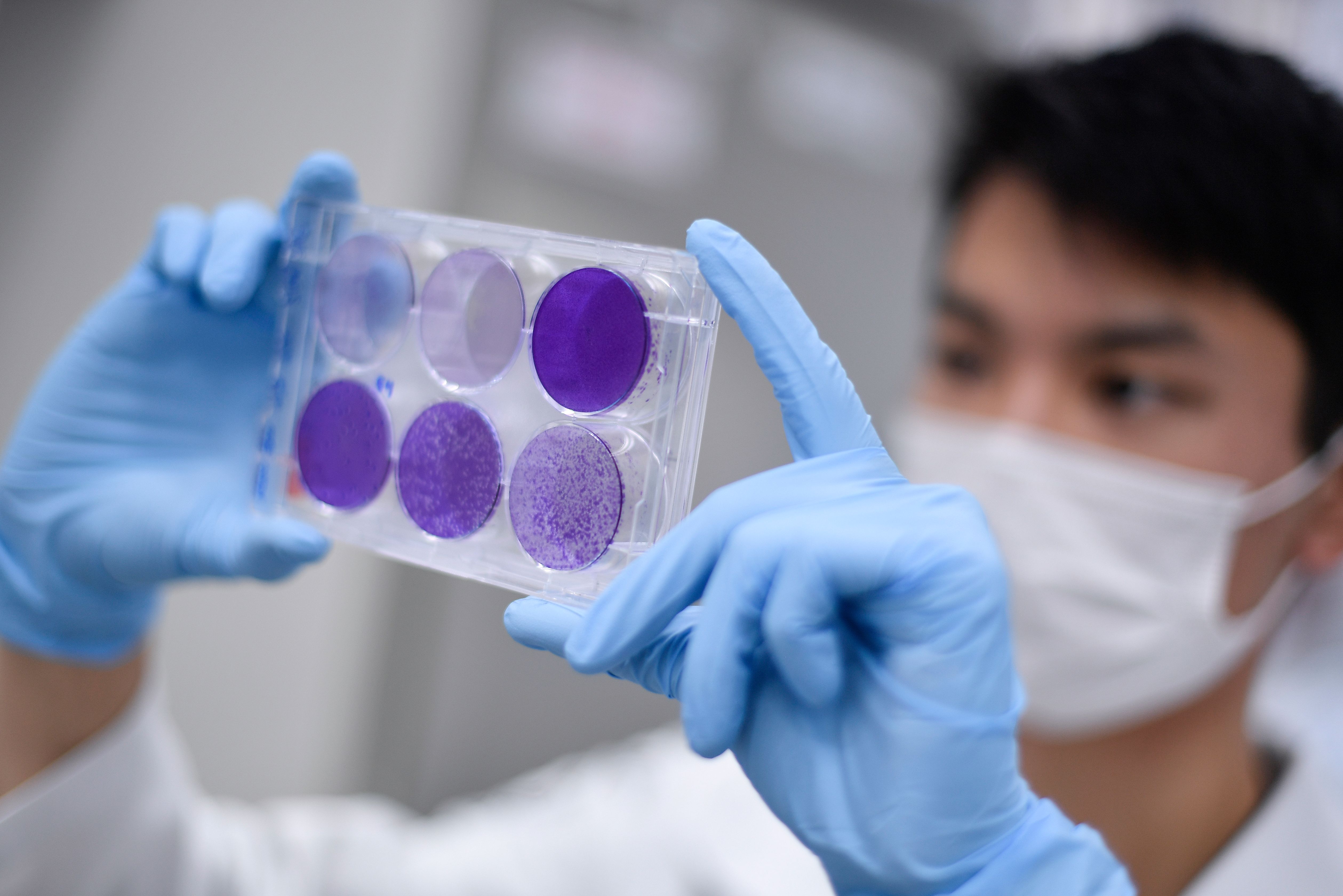
How is a vaccine created?
There are no existing vaccines for coronaviruses, but new technology is accelerating the process; three hours after China published the COVID-19 genome, Inovio Pharmaceuticals in San Diego used a computer algorithm to produce a vaccine blueprint. Preventive vaccines use dead or weakened pathogens to prime the immune system to fight diseases — in the case of COVID-19, by teaching it to recognize the coronavirus protein's "spikes" that latch onto cells. That recognition cues white blood cells to produce antibodies that can fight a real infection. Moderna is pursuing an original approach: injecting messenger RNA (mRNA) molecules that encode instructions for building coronavirus-like proteins, so they can be recognized as foreign threats.
A free daily email with the biggest news stories of the day – and the best features from TheWeek.com
How long will testing take?
Clinical trials usually occur in three phases. First, about 50 healthy human volunteers are paid $1,100 each to be injected with a candidate vaccine, and then monitored to see if they produce antibodies without unintended side effects. If that's successful, a few hundred people get the vaccine, and their immune response and side effects are carefully studied. In phase three, several thousand people are tested: Half get the vaccine, half get a placebo; if vaccinated subjects don't get sick or get sick at much lower rates, the vaccine is ready for FDA approval. This all can take eight to 12 months. If and when a coronavirus vaccine is approved, other problems immediately arise: Who gets it first? And who pays for vaccinations if people are uninsured? Manufacturing billions of vaccine doses will take months, and rich nations could hoard limited supplies. Vaccinating every American could cost $165 billion, Time estimates.
What are the top contenders?
Some of the most promising vaccines build on proven science. Janssen, the Belgian pharmaceutical subsidiary of Johnson & Johnson, is developing a vaccine modeled on the successful vaccine for Ebola. Inovio, the San Diego–based company, and Maryland-based Novavax are modeling vaccines on candidates in advanced trials for MERS, a coronavirus disease similar to COVID-19. In China, 1,000 scientists are working on a vaccine and launching more than 200 clinical trials to test everything from anti-flu drugs to ancient Chinese herbal medicine. Moderna's mRNA approach is also being used by the German company CureVac; German government officials accused Trump of trying to poach CureVac scientists and their intellectual property for the exclusive use of the U.S.
What's a realistic timeline?
There are dozens of vaccines in the pipeline, but COVID-19 cases are expected to peak in the U.S. months before any of them is approved. Scientists raced to find vaccines for SARS, in the early 2000s, and MERS, in 2012, only to shelve their work when those outbreaks were contained. Experts have grimmer expectations for the longevity of coronavirus, meaning a vaccine ready a year from now could still save many millions of lives. With a large number of people getting sick and dying, the race for a vaccine requires a painful amount of patience. "I'm going to bed thinking we made some progress," Moderna president Stephen Hoge says, "and waking up every morning feeling further and further behind."
Promising treatments
A treatment that lessens the impact of COVID-19 is expected to come before a vaccine, but doctors on the front lines warn against high hopes. "We have no idea what works or does not at this point," says Andre Kalil, an infectious-disease physician at the University of Nebraska Medical Center. Kalil is leading U.S. clinical trials for one of the most promising treatments, the antiviral drug remdesivir, which was developed for Ebola. In February, an American passenger on the Diamond Princess cruise ship who contracted coronavirus after the ship docked in Japan became Kalil's first volunteer. Other antivirals being researched are already in use for HIV and malaria. Other tests focus on drugs for lung inflammations, and antibody-based treatments, including using antibody-rich blood serum taken from coronavirus survivors. A survivor can spare enough serum for one to 10 people. A Johns Hopkins University team got FDA approval in mid-March to test this approach. "This is real," team leader Arturo Casadevall says. "In eight weeks, we may have something that's useful."
This article was first published in the latest issue of The Week magazine. If you want to read more like it, try the magazine for a month here.
-
 Political cartoons for February 20
Political cartoons for February 20Cartoons Friday’s political cartoons include just the ice, winter games, and more
-
 Sepsis ‘breakthrough’: the world’s first targeted treatment?
Sepsis ‘breakthrough’: the world’s first targeted treatment?The Explainer New drug could reverse effects of sepsis, rather than trying to treat infection with antibiotics
-
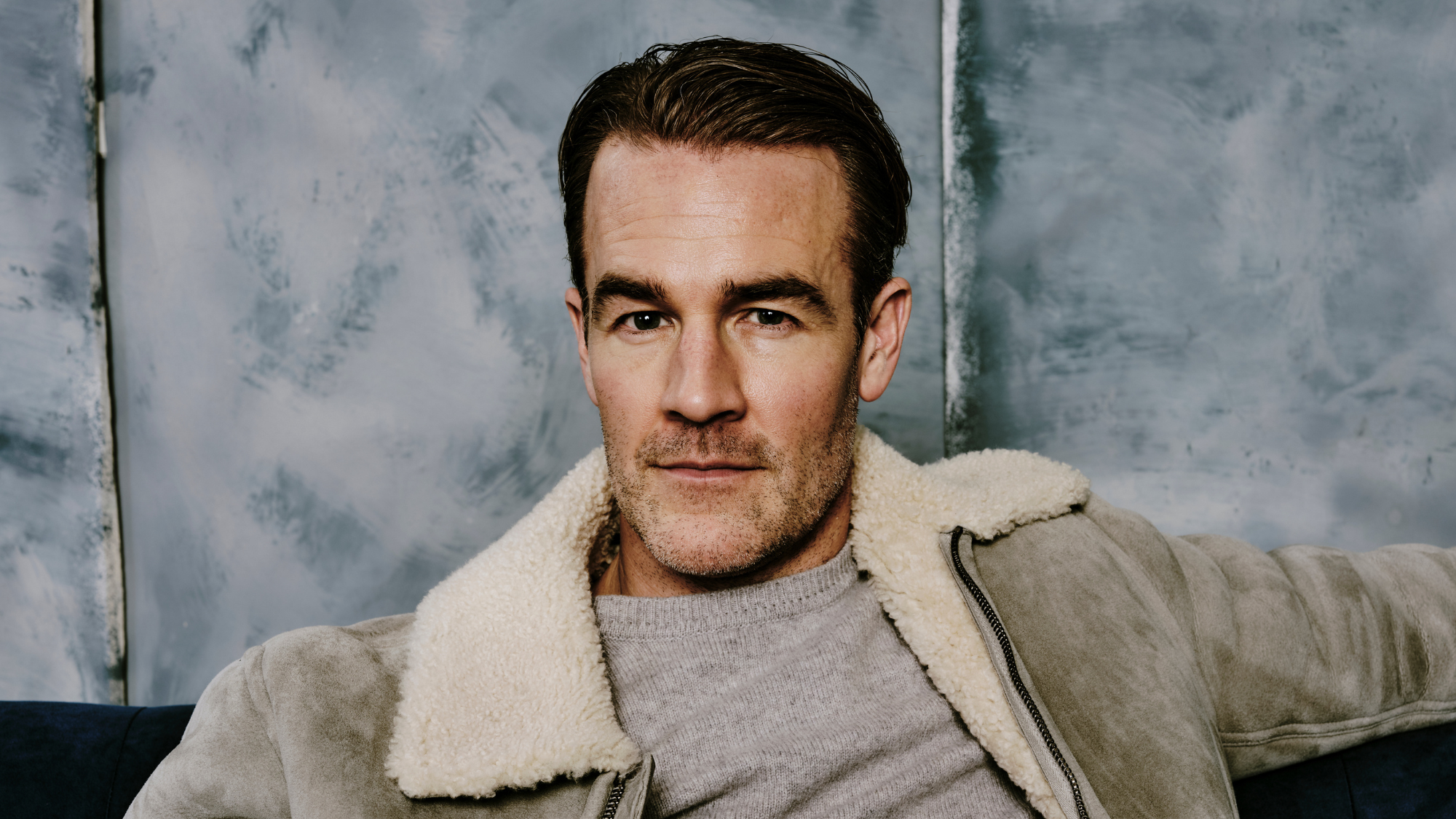 James Van Der Beek obituary: fresh-faced Dawson’s Creek star
James Van Der Beek obituary: fresh-faced Dawson’s Creek starIn The Spotlight Van Der Beek fronted one of the most successful teen dramas of the 90s – but his Dawson fame proved a double-edged sword
-
 A Nipah virus outbreak in India has brought back Covid-era surveillance
A Nipah virus outbreak in India has brought back Covid-era surveillanceUnder the radar The disease can spread through animals and humans
-
 Covid-19 mRNA vaccines could help fight cancer
Covid-19 mRNA vaccines could help fight cancerUnder the radar They boost the immune system
-
 The new Stratus Covid strain – and why it’s on the rise
The new Stratus Covid strain – and why it’s on the riseThe Explainer ‘No evidence’ new variant is more dangerous or that vaccines won’t work against it, say UK health experts
-
 RFK Jr. vaccine panel advises restricting MMRV shot
RFK Jr. vaccine panel advises restricting MMRV shotSpeed Read The committee voted to restrict access to a childhood vaccine against chickenpox
-
 RFK Jr. scraps Covid shots for pregnant women, kids
RFK Jr. scraps Covid shots for pregnant women, kidsSpeed Read The Health Secretary announced a policy change without informing CDC officials
-
 New FDA chiefs limit Covid-19 shots to elderly, sick
New FDA chiefs limit Covid-19 shots to elderly, sickspeed read The FDA set stricter approval standards for booster shots
-
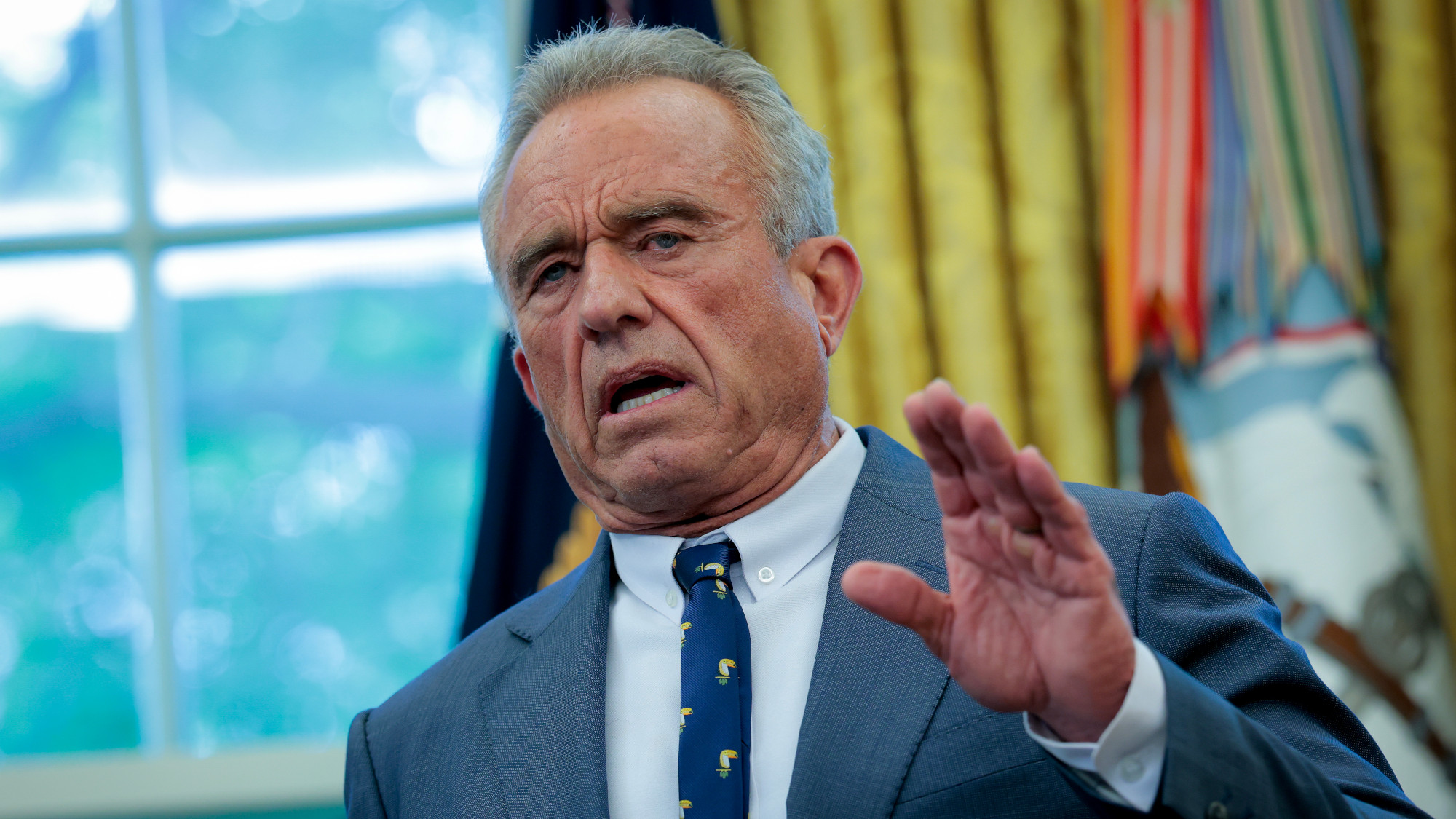 RFK Jr.: A new plan for sabotaging vaccines
RFK Jr.: A new plan for sabotaging vaccinesFeature The Health Secretary announced changes to vaccine testing and asks Americans to 'do your own research'
-
 Five years on: How Covid changed everything
Five years on: How Covid changed everythingFeature We seem to have collectively forgotten Covid’s horrors, but they have completely reshaped politics